Pocket Nurse
Pocket Nurse is a US-based company that makes and distributes medical supplies and equipment for healthcare simulation and education in medicine, nursing, EMS, pharmacy and other allied health groups. The company’s products are extensively used in nursing simulation, but have application across the entire range of the medical simulation industry.
Pocket Nurse began business in 1992 with one product, the Pocket Organizer. This organizer was so popular, the solution led the way to the production and sale of over 5600 products which now includes manikins from Laerdal, moulage tools, and headwalls. The company was founded and owned by a nurse, Anthony Battaglia — who still oversees the company to this day.
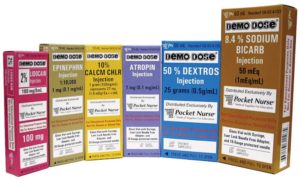
One of Pocket Nurse’s most popular product lines is their Demo Dose medications. The company has been consistently willing to create new practice medications and packaging to match changing clinical practice. Medical simulation should mimic real life situations as much as possible as this adds fidelity to simulation scenarios. Having medications and packages that closely resemble actual medications used in practice provides familiarity for learners which in turn, helps them transition from the classroom to clinical practice.
Sponsored Content:
Medications available include antibiotics, code drugs, chemotherapy, insulins, and vaccines. Unlabeled vials, tablets, capsules, topicals, inhalants and liquids are available for students to practice drawing up and administering various medications. Injectables, irrigation solutions, IV bags and inhalants are also obtainable. Special collections of medications are available e.g. oral foil sample packs and code medications. Pocket nurse distributes medication dispensing systems such as Med Dispense Medication Dispensing Systems and Omnicell.
HealthySimulation.com is dedicated to providing the latest Pocket Nurse news and Nursing Simulation resources from around the world. To follow along, sign up for our free medical simulation email newsletter, follow @HealthySim on Twitter and @HealthySim on Facebook, or join our HealthySim LinkedIn Group!
A variety of blood products are manufactured. These products include packed red blood cells, platelets, fresh frozen plasma and albumin. All the products come with lifelike labels and in a variety of blood groups.
Every institution, whether it be an actual hospital, medical center, long term care facility or educational program must decide whether to use actual medications for practice or products manufactured by companies like Pocket Nurse who deliberately change the name of medications. Thus, digoxin (Lanoxin) becomes digoxn (Lanoxn) and lorazepam (Ativan) becomes Lorazepm (Ativn). These “fake” medications are harmless, non-active formularies that are strictly to be used for practice.
Sponsored Content:
If any of these fake medications ends up in patient areas, Pocket Nurse hopes to alert practitioners if they are not giving the correct medication by the incorrectly spelling the drug name and with the addition of a label “not for human or animal use.” There are cases in the literature where fake meds were given to patients by mistake. In addition, using real medications in educational settings could put learners in jeopardy since exposure to real meds could have a pharmacological effect on the learners themselves, for example, topical or inhaled medications such as nitroglycerin or Ventolin.
Pocket Nurse supplies a large variety of diagnostic equipment such as stethoscopes, blood pressure cuffs, skinfold calipers, otoscopes, mounted diagnostic station and urine analyzers. The company also produces and distributes hospital furniture such as beds, stretchers and a variety of headwalls with oxygen outlets, suction and diagnostic equipment. Infection control products including personal protective equipment are available along with an extensive collection of patient care products.
A collection of obstetric and pediatric products is available as well as surgical equipment such as instruments and suture kits. Educational charts and books, moulage kits and educational models are sold. Patient Simulators, which come in a wide variety of shapes, sizes and prices, include simple models for injections, task trainers, CPR manikins, and whole-body manikins by Simulaids. Pocket Nurse sells totes which contain a collection of their products suitable for specific healthcare professions such as nursing students, nurse practitioners and physician assistants. Educational schools save time by requiring students to purchase these packs. Students find them helpful because they have everything they need for their course of study in a convenient handy pack.
Click Here to Connect to Leading Simulation Vendors like Pocket Nurse!
Pocket Nurse has been the go-to company for nursing and allied health programs for many years. And since the company continues to innovate and adapt to the learning needs of healthcare professions, Pocket Nurse will likely be around for many years to come. The company attends many healthcare simulation conferences like IMSH, and is a key sponsor of INACSL and SimGHOSTS.
Pocket Nurse Latest News

Massive Upload of Must-See IMSH 2024 Exhibitor Demo Videos

Pocket Nurse Acquires DiaMedical USA – Both Companies to Maintain Branding

Medication Management Education: Pocket Nurse Working to Reduce Errors

INACSL 2022 Sim Media Center HealthySimulation.com Interviews – Part I

Pocket Nurse Offers New Design Services for Healthcare Education Construction and Renovation Planning
Demo Dose Disposable Insulin Pen Trainer Ideal for Diabetic Education

Latest Clinical Simulation News From Around the World | December 2021

Pocket Nurse Healthcare Simulation Products Prepare Learners for Bariatric Patients
Injecting Realism: A Closer Look at Demo Dose Simulated Medications

Healthcare Simulation’s Refurbished Simulator Market Takes Off
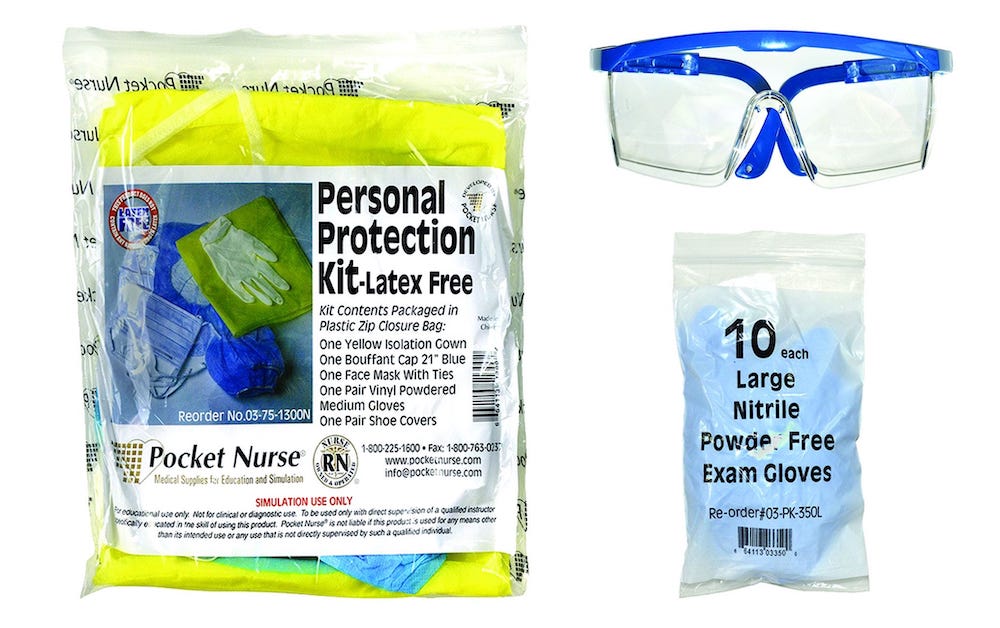
Pocket Nurse: Keys to Patient Safety Include Infection Control & Simulation Education
Sponsored Content: