Pocket Nurse: Keys to Patient Safety Include Infection Control & Simulation Education
A leading manufacturer and distributor of medical supplies, clinical simulation equipment and healthcare education, Pocket Nurse believes that promoting infection control and healthcare simulation education are the keys to a full commitment to patient safety. These factors ultimately contribute to better patient outcomes, while protecting healthcare learners and professionals, because infection control stems from standard precautions based on assessed risk. In this article, Pocket Nurse Content Specialist Dawn Patton Mangine explains how to successfully run a clinical simulation while maintaining infection control, sanitization and safety best practices.
First, learners and educators should understand that infection control principles make use of common-sense practice and personal protective equipment (PPE). Standard precautions are used in all patient care settings and in healthcare educational settings. Everyone should be well aware of the crucial importance of hand hygiene, especially in the current COVID-19 times. In addition, learners, educators, and healthcare workers (HCWs) should understand the basics of using PPE, safe handling and disposal of sharps, and cleaning and disinfecting equipment.
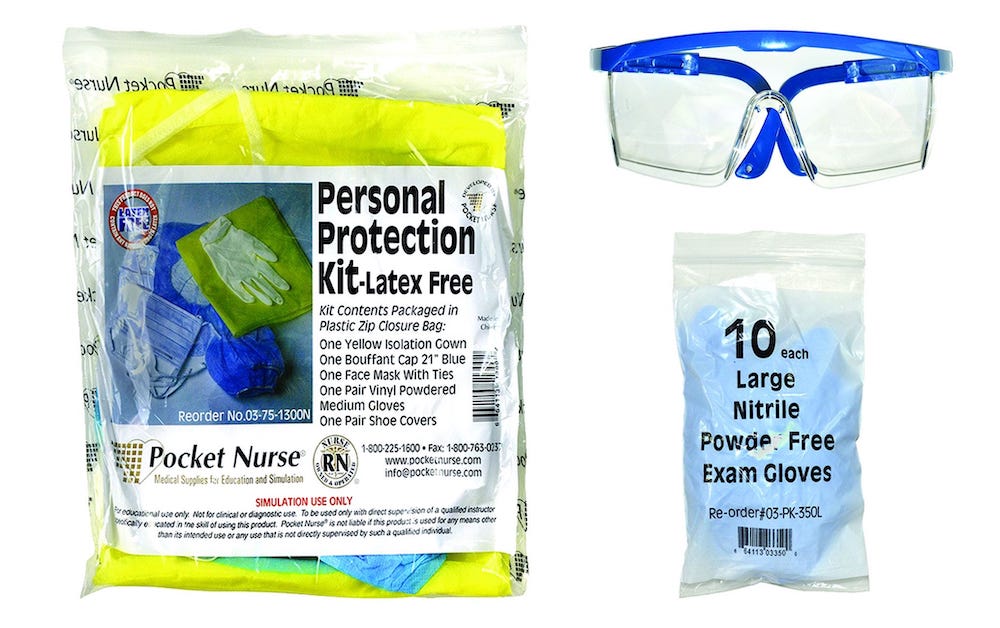
PPE includes disposable gloves, face masks, gowns, goggles and visors, as well as shoe covers and caps where indicated. While the primary purpose of PPE is to protect users from cross-infection, the equipment is also used when handling hazardous chemicals and some types of pharmaceuticals. PPE must be used whenever there is a chance of possible exposure to infectious materials, including airborne particles.
Sponsored Content:
When PPE is included with products, such as CPR masks or any type of diagnostic tools, learners and educators should be sure to use the equipment according to the manufacturer’s directions. Otherwise, they must defer to their institution’s protocol for appropriate use of PPE.
Safe Handling and Disposal of Sharps
Sharps include scalpels, needles, glass ampules, and any type of sharp instrument used in healthcare. According to the Centers for Disease Control and Prevention (CDC), approximately 385,000 needle-stick and sharps-related injuries are received by hospital-based HCWs annually — that is more than 1,000 injuries daily. That number doesn’t include other sharps-related injuries that occur in other clinical and healthcare settings.
Although sharps injuries are associated with the transmission of hepatitis B, hepatitis C and human immunodeficiency viruses (HBV, HCV, and HIV, respectively), sharps injuries have been implicated in the transmission of 20 other pathogens. To reduce the risk of injury and exposure to blood-borne viruses, sharps must be used safely and disposed of carefully. Instructors and employers should provide targeted education and awareness training for all healthcare workers. A plan for safely using and disposing of sharps is vital to the health of HCWs, and teaching safe disposal should be an integral part of healthcare education, especially nursing.
Sponsored Content:
Cleaning and Disinfecting of Equipment
During a localized epidemic, the use of disposable diagnostic tools can be encouraged, even required. One-time use of equipment clearly prevents cross-infection. In general, options and availability have expanded in this area in order to make the use of disposables more affordable. However, in an ongoing pandemic, disposable diagnostic tools may not be cost-effective for organizations.
Companies can address this obstacle by developing non-contact reusables, such as non-contact thermometers, or making the devices easier to clean, such as a one-piece blood pressure cuff. Another option for preventing infection is by thoroughly cleaning and disinfecting tools, patient rooms, and other environments and equipment used in patient care.
Cleaning and disinfecting are two distinct steps in the process for ensuring infection control. Cleaning is the process by which dirt, germs and impurities are removed from a surface. Cleaning doesn’t kill germs — the process simply removes them from a surface, making germs less likely to spread through contact with that surface. While cleaning can reduce infection risk, disinfecting tools and surfaces after cleaning is a vital step.
Disinfecting is the use of chemical agents to kill bacteria, viruses, and other germs on surfaces. In the United States, disinfecting agents approved by the Environmental Protection Agency (EPA) to effectively kill germs are registered by the agency and on List N for easy reference. Sterilization usually incorporates heat to further disinfect tools and devices. This final step ensures an object is free from microorganisms, including bacterial spores. Decontamination, which encompasses cleaning, disinfection and sterilization, ensures that a reusable medical device is safe to use again.
Users should always read the instructions for use (IFU) that come with any device, medical product or educational tool. This is important not just to inform people how to achieve the right level of cleanliness for individual products, but also to ensure they don’t damage equipment by using the wrong type of solutions or processes. Most healthcare equipment companies make these IFUs available on their websites so people can access the information, even if they’ve lost the original documents.
5 Strategies for Simulation Safety
Healthcare simulation education in a safe, controlled simulation environment has been cited as a leading approach in improving patient outcomes, which improves patient safety. Safe care starts in the classroom. However, educators need to be aware that while the use of clinical simulation is imperative to patient safety, educational scenarios need their own set of safety rules.
Quality infection control, innovative simulation education with the right product solutions, and a commitment to patient safety are the ideal mix to ensure a long and healthy future for learners, educators and patients. Here are five strategies all healthcare simulation educators should include across learning environments:
- Clearly label all equipment, supplies, and clinically-simulated medications with information that such equipment, supplies and simulated medications are for educational use only, and not for human, animal or diagnostic use.
- Programs should inform participants, including students and standardized patients, about potential hazards that result from simulation exercises. Every care should be taken to ensure these hazards are minimized.
- Programs that use healthcare simulation must periodically review simulation-related products, solutions, facilities and scenarios to ensure safety. Any potential threats need to be immediately mitigated.
- Educators, staff and faculty must be vetted to ensure they do not mistakenly convey incorrect information, do not treat controversial subjects as certain facts, or neglect to address incorrect actions in debriefing sessions.
- Educators, staff and faculty must adhere to clinical simulation scenarios that are rigorously realistic. The use of “shortcuts” in healthcare simulation (not wearing gloves, not engaging needle guards properly) can give learners a false sense of safety that will adversely affect real patients.
- Simulated medication (such as Demo Dose simulated medications) and IV fluids are two cornerstones of educating students safely and effectively. Demo Dose packaging and labeling are realistic, which helps learners identify the proper medication for treatment. With more than 400 vials, ampules, oral medications, IV fluids, and simulated blood and plasma products, educators can create realistic scenarios such as:
- Transfusion and trauma
- Medication management
- Injection and IV starts
- Advanced Cardiovascular Life Support (ACLS)
- Pharmacy skills and pill counting
More About Pocket Nurse
Pocket Nurse is a U.S.-based company that makes and distributes medical supplies and equipment for healthcare simulation and education in medicine, nursing, EMS, pharmacy and other allied health groups. The company’s products are extensively used in nursing simulation, but have applications across the entire range of the medical simulation industry.
The Pocket Nurse business began in 1992 with one product, the Pocket Organizer. This organizer was so popular, the solution led the way to the production and sale of over 5,600 products, which now include mannequins from Laerdal, moulage tools and headwalls. The company was founded and owned by a nurse, Anthony Battaglia, who continues to oversee the company.
Today, Pocket Nurse supplies a large variety of diagnostic equipment such as stethoscopes, blood pressure cuffs, skinfold calipers, otoscopes, mounted diagnostic stations and urine analyzers. The company also produces and distributes hospital furniture such as beds, stretchers and a variety of headwalls with oxygen outlets, suction and diagnostic equipment. Infection control products including personal protective equipment are available, along with an extensive collection of patient care products.
Learn More About Pocket Nurse
Today’s article was guest authored by Dawn Patton Mangine, Content Specialist at Pocket Nurse.
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!
Dawn Patton Mangine is Content Manager for Pocket Nurse, a leading manufacturer and distributor of healthcare simulation education supplies. Dawn has been with Pocket Nurse since April of 2016. As content manager, she has created and manages SimTalk Blog, a space for topics on simulation and healthcare education. She also curates the Pocket Nurse Twitter and Instagram feeds. Dawn is a creator and story teller, and lives in Pittsburgh with her family (husband, three children, and one dog.)
Sponsored Content: