Learning from the History of Clinical Simulation
The history of clinical simulation is interesting — offering all the intrigue of a world at the intersection of learning theory, innovative technology, patient safety and care. Whereas the tour-de-force that led to the widespread use of healthcare simulation was based in the patient safety movement, one can look back further to see its earlier origins in aviation. Perhaps the greatest value that the history of simulation in healthcare provides is insight into some powerful lessons. A strong understanding of medical simulation’s past can help modern day simulationists understand plan for the future of their clinical simulation programs. This understanding can also help simulation educators and administrators ask the right questions, learn from other disciplines and think about different ways to accomplish their goals.
Simulation in Healthcare: Beginnings Elsewhere
Considering the potential to improve patient care and save lives, one might think that the practice of simulation originated in healthcare. The staggering number of deaths due to medical error worldwide would appear to be the match that lit the fire of the patient safety movement that sparked widespread use of clinical simulation. After all, 250,000 deaths annually (in the United States alone) are caused by mistakes in healthcare delivery feels egregious. One may easily assume that must be what caused trainers to begin using healthcare simulation!
Sponsored Content:
If only that were the case. Rather, simulation’s initial use (in a safety-focused form that reflects contemporary usage) began in another field entirely — the field of aviation. As early as the 1930s, rudimentary aircraft simulators were being used to train pilots. While not initially popular, the rapidly-developing aviation industry realized in a few short years that there were great lifesaving (and cost-saving!) benefits to simulation. Pilots finally had the chance to practice realistic training scenarios to reduce error when actually in the air. Soon, the use of simulation was widespread when training new pilots or retraining experienced ones, driven by a strong culture of preemptive safety.
Healthcare Simulation Sparks
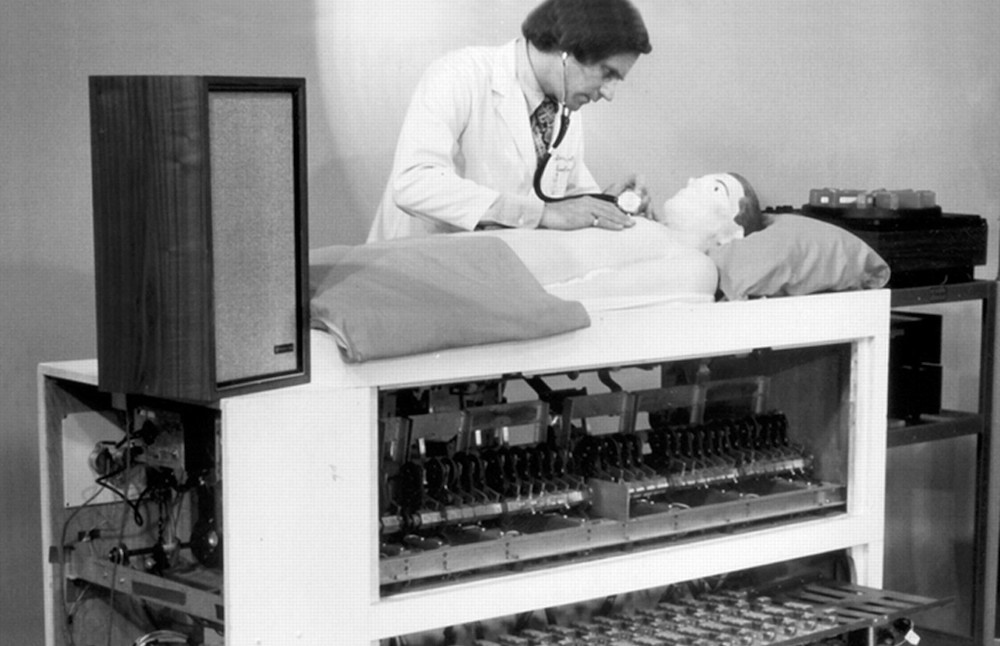
Simulation’s use in healthcare had a few early starts over the past few hundred years — for a detailed view starting as early as 500 BC, HealthySimulation.com Founder Lance Baily highlights the most primitive uses of simulation history in Chapter one of “Comprehensive Healthcare Simulation Operations, Technology, and Innovative Practice.” However, healthcare providers only began to adopt the techniques and practices of medical simulation familiar to clinicians today beginning in the 1960s. The practice of mouth-to-mouth resuscitation had just been developed formally in 1956, and was soon joined by its counterpart, cardiopulmonary resuscitation (CPR), in 1960. Of all individuals, the toy manufacturer Asmund Laerdal, with his strong knowledge of plastics manufacturing, began the production of “simulators” to facilitate the practice of this new life saving procedure. (famously, the face of his Resusci-Anne mannequin was modeled after the Lady of the Seine, whose gentle appearance could decrease the intimidation associated with practicing CPR.)
Sponsored Content:
With the rise of CPR, the healthcare industry began to recognize the power of practice. Nurses and physicians learning this new technique were inspired by seeing the immediate effects on patient lives. Over time, this started to strengthen the popularity of using clinical simulation as a regular part of healthcare training. Early simulationists like Dr. David Gaba and Dr. Stephen Abrahamson, along with manufacturers like Gaumard and CAE Healthcare, also laid the groundwork of medical simulation principles, techniques, and tools. However, a few decades had yet to pass before clinical simulation saw widespread implementation.
The Institute of Medicine’s Effect on Healthcare Simulation
Despite much of the work that had been done to prove the usefulness of healthcare simulation, the practice remained mostly nascent until 1999. This was the year the Institute of Medicine released the report “To Err Is Human: Building a Safer Health System.” One of the main impacts of this paper was to bring to light the reality and devastation of medical errors. But perhaps more importantly, the report called upon change from within the healthcare industry.
Now the stage was set for the world to turn to clinical simulation as a way of reducing error and improving patient safety before reaching the bedside. In the years subsequent to this report, hospitals and academia began in earnest to research and observe the impact that healthcare simulation had on the spectrum of care.
Lessons to be Learned from Healthcare Simulation’s Past
If there is one tenet at the center of clinical simulation, it’s the opportunity to learn from decisions made. Typically, this is the learner gaining an understanding of their own choices; but in this case, the history of the use of healthcare simulation can provide a few valuable lessons. This is true not only for simulation educators, but for everyone involved in the chain of healthcare training and delivery.
Do Something Different: Healthcare has been around a long time. There are positive aspects to this, such as having millennia to build deep knowledge of illness and the human body. However, this also increases the likelihood of entrenched practices, for better or for worse. Nurses, doctors and other healthcare providers practiced experiential learning the same way for hundreds of years — with real patients! To move toward new attitudes in patient safety, this required clinicians to have the willingness to do things differently than they had done before.
Think Outside the Bed: A fascinating lesson is how much the healthcare industry was able to learn by taking a cue from the emerging discipline of aviation. As innovative technologies are generated each day and new industries crop up every year, how much can healthcare providers learn from fields they may not typically involve themselves in? Can healthcare learn lessons from the fields of artificial intelligence, robotics, or blockchain technology?
Ask the Right Questions (Especially if They’re Hard!): One of the most powerful aspects of clinical simulation (due to the focus on debriefing) is the inherent potential to create a culture of inquiry. healthcare providers began asking if the current way of training clinicians was sufficient. While uncomfortable and demanding of change, these questions led to sweeping changes in training and improvement of care, that patients reap the benefits of today. As a modern example, a nurse educator may ask whether the minimum program accreditation standards adequately prepare her learners for practice, or whether she should establish additional structures to promote their independence as future nurses.
History serves many purposes, but the realm of healthcare history depicts lessons that can improve patient care, if listened to attentively. Clinical simulation, with a unique combination of innovation and learning, has had a unique part to play in the history of healthcare training. And while that history is entertaining, the modern simulationist can make use of the past for more than just amusement. Like a wise mentor, that past can serve to teach lessons that would not otherwise be evident.
Learn More About Clinical Simulation
Nathan Costiuc, MSN, APRN, FNP-BC, is a Nurse Practitioner and Healthcare Simulation Educator. He began his career delivering clinical simulation to nursing students, quickly realizing the industry’s potential to impact modern training for all healthcare professionals. In navigating better ways to deliver clinical simulation, Costiuc entered into the world of virtual reality, and now works as a Clinical Education Specialist for Oxford Medical Simulation. His passion is in using innovative methods and emerging technologies to reduce medical error, solve practical problems, and improve patient care. He also actively works with disabled veterans in the clinical setting.
Sponsored Content: