In Situ Simulation Prepares Rapid Response Teams at Gordon Center
Rapid response teams (RRTs), an integral part of a hospital’s rapid response service, are a focus area for medical training at the Gordon Center for Simulation and Innovation in Medical Education at the University of Miami Miller School of Medicine. The institution conducted the first in situ training at Bascom Palmer Eye Institute in 2013 and, since then, has planned and executed almost 100 trainings within the University of Miami and beyond. RRTs, such as those of the Gordon Center, care for patients, family members and even staff who experience a medical crisis at a hospital, often before or after being seen by a physician or care provider.
“At the University of Miami, we take the education and training of our rapid response teams very seriously,” said Assistant Director of the Gordon Center and Director of the Prehospital and Emergency Healthcare Division Ivette Motola, M.D., MPH. “We want to make sure that our rapid response team members are well prepared for any situation they may find themselves in and know the processes and procedures well enough so they can take necessary action promptly and ensure the best outcomes for our patients. Ultimately, that should be the goal of every rapid response team.”
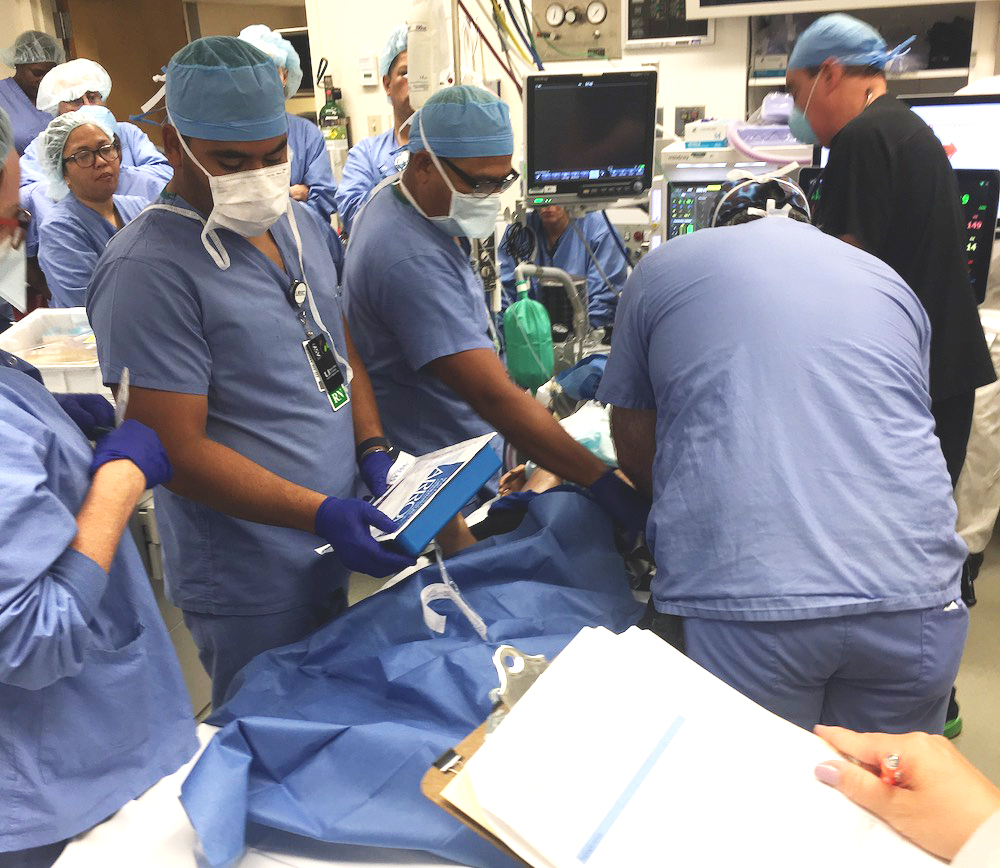
RRT adoption is a Joint Commission requirement that enables hospital or clinic staff members to obtain help from experts when a patient’s condition deteriorates. To ensure consistent training and quality across UHealth – the University of Miami Health System, the Gordon Center developed an “in situ” quarterly RRT training. With patient safety as their central objective, these critical event simulations take place in the medical team’s natural setting and include pre-op, OR, post-op, outpatient clinic, ICU and medical-surgical floor teams. They are conducted without giving the RRT members at the various hospitals and clinics prior notice or preparation time, just as would be the case in a real-world scenario.
Sponsored Content:
“These trainings are unannounced for a reason,” said Motola. “We usually inform and prepare the training together with the health system education team and nurse manager or charge nurse, but that’s it. While most rapid response training is done in simulation labs or other highly controlled environments, our training is designed to be conducted where actual rapid response events occur, hence the term ‘in situ.’ We aim to make the training as realistic as possible, and the element of surprise, combined with being in the actual clinical environment where responses occur, make it as realistic and high-fidelity as possible.”
The United States’ oldest and most established medical simulation center, the Gordon Center has a team of experts visit hospitals and departments within UHealth with a simulated situation as part of training. The teams being trained primarily consist of nurses, nurse practitioners, residents, physicians and other medical and ancillary staff usually involved in a response, which is another key feature.
When they are called to the training, RRT members do not know right away that the clinical simulation is not a real situation or emergency. The chosen simulations reflect circumstances that could occur at the hospital, clinic or department where RRTs are trained. The cases include various emergency events such as a patient passing out in the waiting room or an anaphylactic shock in an MRI machine.
“At the end of each training, there is a debriefing among everyone involved, and we compile and share a written report,” said Motola. “The focus of these debriefs is on clinical content, teamwork and system effectiveness.”
Sponsored Content:
During the training, Gordon Center educators discuss questions with the RRTs that address algorithms followed, equipment available, equipment used and effective teamwork strategies. Through the in situ training and the following debriefs, the Gordon Center team can assess the learners (RRT members) and the systems as well as test new equipment, spaces or processes.
Since these trainings occur on a quarterly basis, the Gordon Center alternates healthcare simulation scenarios and compares them with previous training scenarios to track the team’s progress. Common findings have included reduced response times, improved confidence among the rapid response team members and better familiarity with low-frequency incidents.
The outcomes of this training have shown to be more impactful and the skills learned more internalized than those done in artificial and planned environments that gave RRT members time to prepare for a simulation. In situ training thus ensures the highest levels of patient safety throughout the health system in settings where patients have not yet been seen by physicians.
“Trainings of this sort are necessary across all types of hospitals and clinics as patient emergencies can happen anywhere,” said Motola. “In fact, we are seeing in situ simulations being done at more and more hospitals and health systems across the country and the globe. Even the very best hospitals need them. For example, teams at Bascom Palmer Eye Institute, the nation’s leading ophthalmology hospital, are a regular part of our training. This illustrates that even the leading hospitals need rapid response training.”
Learn More About The Gordon Center
Lance Baily, BA, EMT-B, is the Founder & CEO of HealthySimulation.com, which he started while serving as the Director of the Nevada System of Higher Education’s Clinical Simulation Center of Las Vegas back in 2010. Lance is also the Founder and acting Advisor to the Board of SimGHOSTS.org, the world’s only non-profit organization dedicated to supporting professionals operating healthcare simulation technologies. His co-edited Book: “Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice” is cited as a key source for professional certification in the industry. Lance’s background also includes serving as a Simulation Technology Specialist for the LA Community College District, EMS fire fighting, Hollywood movie production, rescue diving, and global travel. He and his wife Abigail Baily, PhD live in Las Vegas, Nevada with their two amazing daughters.
Sponsored Content: