How to to Start a Faculty Development Program in Medical Simulation
Faculty development is a key part of any academic program and medical simulation is no different. As an emerging field, Healthcare Simulation continues to evolve rapidly with new technologies and methodologies being released every month. As such, building an effective faculty development program allows institutions to ensure their teams stay up to date with the latest research supported trends, community identified best practices, and innovative technologies. This HealthySimulation.com article will outline the purpose behind a faculty development program in clinical simulation, share three key considerations when developing such a program, and review ways to gain crucial administrative support.
The International Nursing Association for Clinical Simulation and Learning (INACSL) has created community standards of best practice, which include breakdowns of key components necessary for clinical educational and training institutions to be successful with simulation adoption and utilization. These standards include one specifically addressing professional development which states “As the practice of simulation-based education grows [within an institution], professional development allows the simulationist to stay current with new knowledge, provide high-quality simulation experiences, and meet the educational needs of the learners. This standard helps inform faculty decision-making with regards to other healthcare simulation standards of best practice, including scenario design, simulation facilitation, session debriefing and professional integrity, among others.
Three key considerations for establishing a clinical simulation faculty development program revolve around scenario design, simulation operations, and learner session debriefing. For example, when designing a new medical simulation scenario, faculty must be aware of the andragogy of best practices for scenario design. This includes considerations for constructing measurable objectives that build upon the learner’s foundational knowledge, using various types of fidelity to create the required perception of realism, pilot testing simulation-based experiences before full implementation, and many more. Without this knowledge, clinical educators may design scenarios which fail to demonstrate performance improvement outcomes as they relate to clinical simulation program goals.
Sponsored Content:
For example, when the learning objectives include performing detailed neurological physical examinations, utilizing a simulated patient may be a better medium over the selection of a high-fidelity manikin. As all simulation-based experiences require purposeful and systematic yet flexible and cyclical planning, faculty must receive specialized professional development in order to maximize the effectiveness of your simulation activities. Faculty can only achieve effective learning objectives on a consistent basis after understanding how their individually designed scenarios connect to the larger program goals.
Understanding the Unique Needs of Healthcare Simulation Operations
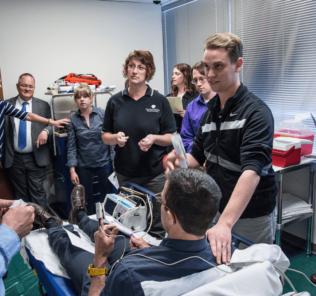
The next thing to consider when starting a faculty development program in medical simulation is the operation of the healthcare simulation scenario itself. Depending on what the goals or learning objectives of the session are will determine what medium of healthcare simulation to use. Faculty involved in teaching using medical simulation need to be aware of how to utilize or operate inside each of these mediums.
Often faculty think something like a simulated patient (SP) does not need extra training because SP’s are just humans playing a role or patient.This may be because faculty interacts with real patients so frequently they may assume that those experiences translate naturally into a case where an SP is involved. But this is not the case. Simulated patients are highly trained and an integral part of any healthcare simulation that involves them. Training a simulated patient on the various aspects of the case ensures a more realistic performance from the SP that increases the value offered to the learners. This concept of increasing realism can be applied to any medium of medical simulation training.
Sponsored Content:
If a task-trainer is being used there may be certain aspects of the trainer that are not completely analogous to how a procedure is performed in reality. These differences from real life are important to make faculty aware of and allowing faculty the opportunity to train on the task trainers they will be utilizing ensures quality of teaching remains high.This allows the faculty to be able to convey the variances from reality that the task trainer may require. An example of would be a simulated IV arm that does not have pulses, or a birthing mannequin that needs the baby to be disengaged from the manikin before completing delivery. Faculty with the ability to explain these differences ahead of time allows the faculty to gain more trust from the learners and ensures that the learners are prepared for how the skills may be done on future patients.
Many medical simulation labs have Healthcare Simulation Technology Specialists (Sim Techs), aka Healthcare Simulation Operations Specialists, highly trained employees who specialize in managing the technical aspects of medical simulation. But not every clinical simulation program will have access to the resources necessary to hire such an operational specialist. Regardless of team dynamics, every healthcare simulation educator should understand the core functionality of the simulation technologies available, and their basic operation. Any institution preparing to adopt clinical simulation technologies, should be prepared to provide faculty development in the core functionality of available simulated systems. Without this knowledge, faculty are limited in their ability to conduct medical simulation sessions to the fullest potential and reduce their capacity to fully evaluate course outcomes. Learn more about operating simulation technologies from the SimGHOSTS non-profit organization.
All of the largest global manikin manufacturers have online guides on how best to utilize their individual applications to design custom scenarios, modify pre-built scenarios, or operate medical simulation experiences ‘on-the-fly’. When possible, involve the Operational Specialist in the design of clinical simulation scenarios to ensure that expected technological outcomes occur without technical assistance during the live experience.
One final consideration to empower clinical faculty to execute successful simulation experiences is to standardize the debriefing facilitation process. Research shows that the majority of clinical knowledge gained from healthcare simulation occurs inside a structured debriefing environment, after the simulated experience concludes. Faculty must be made aware that following strict policies and frameworks around the debriefing process facilitates the greatest possible outcomes. There are several debriefing frameworks that require minimal training and which can aid the novice debriefer to quickly understand how debriefing functions. Simulation Operational Specialists can also be utilized to assist faculty in video assisted debriefing by entering timeline annotations, time stamps, and asynchronous evaluation of the simulated clinical encounter.
Stakeholder and administration considerations should always be accounted for when a faculty development program is being designed in any healthcare simulation lab. Healthcare institutional leadership will expect to see concrete areas of clinical performance improvement amongst the faculty and their respective cohorts who have completed such training programs. Regardless of the evolution of a simulation center’s professional development program, the recommendation is to keep meticulous track of all available data. Core statistics such as hands-on simulation hours, certifications, research findings, performance improvement metrics, and room utilization all contribute to long-term administrative support. There should be no doubt that simulation programs that invest in the professional development of their educational and training faculty will contribute to improved clinical outcomes in a multitude of ways.
Learn More About Simulation Faculty Development Through Our CE Webinars!
Wesley Lockhart, PhD.c, MSMS, CHSE, CHSOS – Wesley has been involved in medical simulation for almost two decades, having started his simulation career as a Standardized Patient throughout high school and college. His first position out of college while preparing for medical school was a simulation technician at UC Riverside, he fell in love with medical simulation and the impact it could have on future providers and their future patients. After deciding against medical school, Wesley pursued a graduate degree in Medical Simulation from Drexel University, received his CHSE and CHSOS from SSH, and is currently a PhD candidate at MGH-IHP. Currently, Wesley works as the Simulation Director at the newly established University of Texas Tyler School of Medicine after 8 years at UC Riverside. His interests in simulation focus on Artificial Intelligence, Virtual Reality, Mastery learning, Debriefing, and integrating simulation into established curricula. Wesley lives in East Texas with his wife Kristen, daughter Sophie, and 3 standard poodles. When not head down in a simulation scenario, Wesley enjoys video games, fantasy novels, escape rooms, and board games with friends.
Sponsored Content: