Physiology: The Force Behind Healthcare Simulation – A Guide for Techs, Part 10B: Heart Blocks
This article is a continuation of a series of articles by Dr. Kim Baily on the Force Behind Healthcare Simulation: Physiology. Part 10B focuses about cardiac dysrhythmias and is designed to provide introductory information for healthcare simulation staff with a limited background in physiology and/or medicine, such as those operating as simulation technicians. Dr. Kim Baily PhD, MSN, RN, CNE, was previously the Simulation Coordinator for Los Angeles Harbor College and Director of Nursing for El Camino College. Over the past 16 years Kim has developed and implemented several college simulation programs and previously chaired the Southern California Simulation Collaborative. The rest of the Physiology Series is linked below!
Basic cardiac function, interpreting cardiac rhythms and atrial dysrhythmias have already been discussed through our previously Physiology articles linked below. This article covers first, second and third degree (complete) heart blocks. Please download this image of rhythm strips and use the following steps to analyze cardiac rhythms:
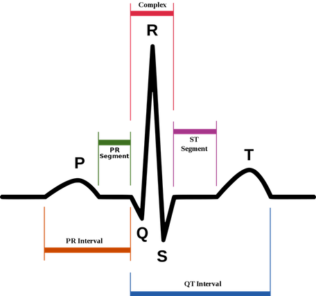
- PR interval: The period of time from the onset of the P wave to the beginning of the QRS complex (contraction of the ventricles).
- Determine rhythm: Does the rhythm have a regular pattern. Is the time between P waves equal and how many P waves occur in one minute. This information yields the atrial contraction rate and its regularity.
- Measure the R to R distance – ventricular rhythm. How many QRS complexes per minute and are they equally spaced.
- Is there one P wave for every QRS or are there extra P waves or QRS complexes?
- Measure intervals and segments including PR interval, ST segment, and QT. Are Q waves present.
Note that on ECG paper, voltage is measured along the vertical axis (10 mm is equal to 1mV in voltage) and the horizontal axis is time (each small square is 0.04 sec and each large square is 0.2 sec). When the heart rate is regular, heart rate can be calculated by dividing 60 by the time between R waves or by counting the number of R waves in a 6 second strip and multiplying by 10.
Sponsored Content:
Cardiac muscle tissue has autorhythmicity which is the unique ability to initiate a cardiac action potential at a fixed rate. Impulses spread rapidly from cell to cell to trigger the contraction of the entire heart. This autorhythmicity is modulated by the endocrine and nervous systems. In the healthy heart, the cardiac rate is set by the Sino-Atrial node (SA) aka the heart’s pacemaker.
The depolarization of the SA node is influenced by the nervous system and circulating molecules such as adrenalin. Atrial cells normally have an intrinsic rate of 60-80bpm, junctional cells (in the AV junction) normally have an intrinsic rate 40- 60bpm and ventricular cells normally have an intrinsic rate 20-40bpm. Without the influence of the SA node and a blocked conduction system, cardiac tissues would contract at the rates above.
When the electrical signal from the SA node spreads out across the atria, they contract. The signal then passes from the atria through the Atrioventricular (AV) node to the ventricles. The AV node acts as a gate causing a very short pause in electrical conduction which allows the atria to contract and empty. Passage through the AV node is reflected in the PR interval on an ECG. Conduction continues down the Bundles of His and Purkinje Fibres in the ventricles which in turn, causes the ventricles to contract.
Heart Blocks: Usually the AV junction slows cardiac conduction just long enough for the atrial to complete contraction. The normal PR interval is less than 0.2 seconds. When conduction through the AV node is delayed the PR interval is prolonged or blocked completely. There are three groups of heart blocks, first degree, second degree and third degree aka complete heart block.
Sponsored Content:
First Degree Heart Block
First-degree atrioventricular (AV) block is defined as a PR interval of greater than 0.20 seconds on electrocardiography (ECG) and without disruption of atrial to ventricular conduction. The SA node is influenced by both sympathetic nervous stimulation “fight or flight” and by the parasympathetic nervous system (rest and digest) via the vagus nerve. In younger healthy adults first degree heart block may be caused by increased vagus nerve stimulation which slows the heart rate and prolongs the PR interval. In older adults the heart block may be caused by fibrosis, coronary heart disease, myocardial infarction, inflammation, infiltrative diseases, and neuromuscular disorders.
Most patients are unaware they have a first degree block and it does not usually require medical intervention however although rare, patients should be checked regularly to make sure the heart block does not progress into a more serious block or an atrial dysrhythmia develops. When the PR interval goes beyond 0.3 seconds patients may become symptomatic – dyspnea, malaise, lightheadedness, chest pain, or even syncope due to poor synchronization of atrial and ventricular contractions.
Second Degree Heart Block
There are two types of second-degree atrioventricular blocks: Mobitz type I, also known as Wenckebach and Mobitz type II.
In Mobitz type I (Wenckebach) the PR interval becomes progressively longer until finally the atrial complex is completely blocked and there is a P wave but no ventricular conduction (QRS). The cycle then repeats itself with longer and longer PR intervals followed by a dropped beat. The prolonged beats followed by dropped beats form a pattern. Patients may be asymptomatic. Mobitz type I may be caused by a high vagal tone (as in Type 1 blocks) or by inferior myocardial ischemia, medication toxicity (AV nodal blocking agents), hyperkalemia, cardiomyopathy (Lyme disease), or following cardiac surgery.
In Mobitz type II there is no prolongation of the PR interval but every so often the P wave is not followed by a QRS complex (i.e. no ventricular contraction). This block may be related to pathophysiology below the AV node within the node infra-nodal conduction system of the ventricles and maybe associated with a widened QRS complex, bundle-branch block, or fascicular block. Technically if more than one P wave is skipped, this rhythm is considered a complete block. This block may be caused by myocardial ischemia and fibrosis The danger of a Mobitz type II block is that it might advance to a complete heart block. Patients with Mobitz type II may present with bradycardia, fatigue, dyspnea, chest pain, presyncope or syncope, and even sudden cardiac arrest.
Third-Degree Atrioventricular Block aka Complete Heart Block
EKG review of a patient with a complete heart block will show no correlation between contraction of the atria and contraction of the ventricles. The P waves march out at one rate while the QRS marches out at another usually much slower rate with no apparent relationship. The QRS complex may be wide since it is not initiated in the AV node. The SA node has lost control of heart rate. Conduction through the AV node is completely blocked and the ventricles beat at their own innate rate (20-40 beats per minute). Since it is the contraction of the ventricles that pushes blood out into the systemic circulation, cardiac output (volume per minute) is greatly reduced.
As with the other blocks, complete heart block may be caused by fibrosis, other cardiac diseases, cardiac surgery, Lyme disease and systemic lupus erythematosus (SLE) as well as certain medications such as antiarrhythmics and digoxin. Patients are often distressed and present with heart failure, respiratory distress, and hypoperfusion such as diaphoresis, tachypnea, altered mental status, retraction, cool skin, and decreased capillary refill.
Complete heart block will require a rapid intervention with temporary pacing followed by surgery to implant a permanent pacemaker. In addition, the patient should be treated for the underlying cause of the complete heart block. Atropine is rarely effective.
The closer healthcare simulation mimics actual clinical situations the better the experience for learners. Symptomatic cardiac blocks require an interprofessional team response. Medical healthcare simulation scenarios lend themselves not only to improve clinicians’ understanding of these cardiac disorders but also as a vehicle to improve team interaction and communication. Healthcare simulation team members who have a limited medical background support simulation in multiple ways however, by increasing their knowledge of physiology, they can more fully contribute to learning activities.
Read the Entire Physiology: The “Force” Behind Healthcare Simulation HealthySimulation.com Article Series:
- Part 1: Blood Pressure
- Part 2: Heart & Respiratory Rate
- Part 3: Pulse Oximetry
- Part 4: Diabetes
- Part 4B: Hypoglycemia & Excel Template for Simulated EHR
- Part 4C: Insulin
- Part 5: Sepsis
- Part 6A: Hypovolemia (Intro)
- Part 6B: Hypovolemia (Treatment & Simulation Tips)
- Part 7A: IV Fluids & Bags
- Part 7B: IV Pumps & Site Access
- Part 7C: PCA for Pain
- Part 8: ABGs
- Part 9: Sepsis Labs
- Part 10:Intro to Cardiac Rhythms
- Part 10A: Abnormal Cardiac Rhythms
Learn More About Heart Block Rhythms!
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!
Dr. Kim Baily, MSN, PhD, RN, CNE has had a passion for healthcare simulation since she pulled her first sim man out of the closet and into the light in 2002. She has been a full-time educator and director of nursing and was responsible for building and implementing two nursing simulation programs at El Camino College and Pasadena City College in Southern California. Dr. Baily is a member of both INACSL and SSH. She serves as a consultant for emerging clinical simulation programs and has previously chaired Southern California Simulation Collaborative, which supports healthcare professionals working in healthcare simulation in both hospitals and academic institutions throughout Southern California. Dr. Baily has taught a variety of nursing and medical simulation-related courses in a variety of forums, such as on-site simulation in healthcare debriefing workshops and online courses. Since retiring from full time teaching, she has written over 100 healthcare simulation educational articles for HealthySimulation.com while traveling around the country via her RV out of California.
Sponsored Content: