Physiology: The Force Behind Healthcare Simulation – A Guide for Techs, Part 11: ARDS
Many healthcare simulation programs are beginning to offer simulations related to the care of COVID-19 patients. Acute Respiratory Distress Syndrome (ARDS) is a common cause of death in COVID-19 patients. The recognition of ARDS and prompt interventions are crucial steps in the care of COVID-19 patients. This article by guest author Dr. Kim Baily PhD, MSN, RN, CNE, previous Simulation Coordinator for Los Angeles Harbor College and Director of Nursing for El Camino College, provides an introduction to the physiology of ARDS for healthcare simulation technicians who may have limited medical experience, and is part of an ongoing series of basic physiology topics in her ongoing series Physiology: The Force Behind Healthcare Simulation – A Guide for Sim Techs (linked below).
According to the CDC, among all patients, a range of 3% to 17% developed ARDS compared to a range of 20% to 42% for hospitalized patients and 67% to 85% for patients admitted to the ICU. Based on a study of over 44,000 persons with COVID-19 from China, the CDC reported that the illness severity can range from mild to critical:
- Mild to moderate (mild symptoms up to mild pneumonia): 81%
- Severe (dyspnea, hypoxia, or >50% lung involvement on imaging): 14%
- Critical (respiratory failure, shock, or multiorgan system dysfunction): 5%
In those patients who developed severe disease, the medium time to dyspnea ranged from 5 to 8 days and the median time to ARDS ranged from 8 to 12 days. Further, patients can rapidly deteriorate one week after illness onset. Among all hospitalized patients, a range of 26% to 32% of patients were admitted to the ICU. Several organizations such as The World Health Organization and the Surviving Sepsis Campaign have offered guidelines for the treatment of COVID-19. Links to these and other articles may be found on the CDC website.
Sponsored Content:
Complications of COVID-19 include pneumonia, hypoxemic respiratory failure/ARDS, sepsis and septic shock, cardiomyopathy and arrhythmia, acute kidney injury, and complications from prolonged hospitalization including secondary bacterial infections.
Basic Lung Physiology and Terminology:
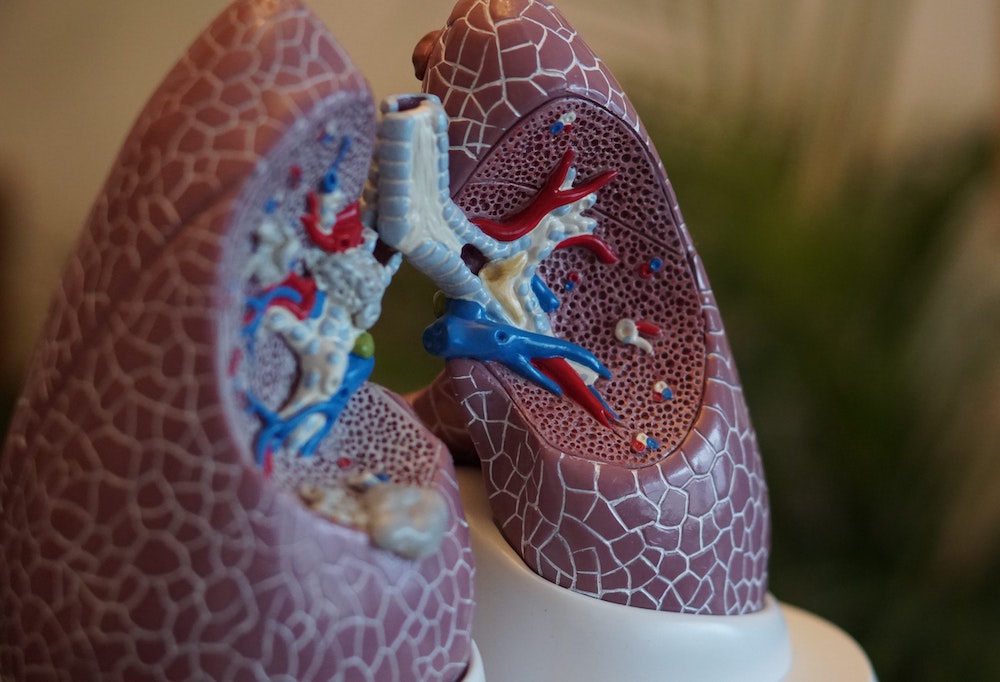
Anatomy: The lungs may be viewed as an upside down tree with the trunk representing the widest airways (trachea and bronchi) at the top and many, many branches that divide into smaller and smaller airways which in turn lead to millions of tiny little sacs (alveoli) where oxygen/carbon dioxide exchange takes place. Keeping the alveoli open is important for gases to be able to move into the alveoli. Type II cells in the alveoli secrete surfactant which lowers the surface tension of the alveoli which in turn helps to keep the air sacs open. The alveoli are lined with a single layer of cells. Capillaries containing blood lie alongside alveoli. A space exists between the alveolus wall and the capillary wall known as the interstitial space. Oxygen crosses the wall of the alveolus, through the interstitial space and capillary cells and finally into the bloodstream. The capillaries collect together to form the left pulmonary vein which brings oxygenated blood to the left side of the heart. The left ventricle pumps blood to the entire body. Note that as oxygen moves from the alveoli into the circulation, carbon dioxide moves in the opposite direction.
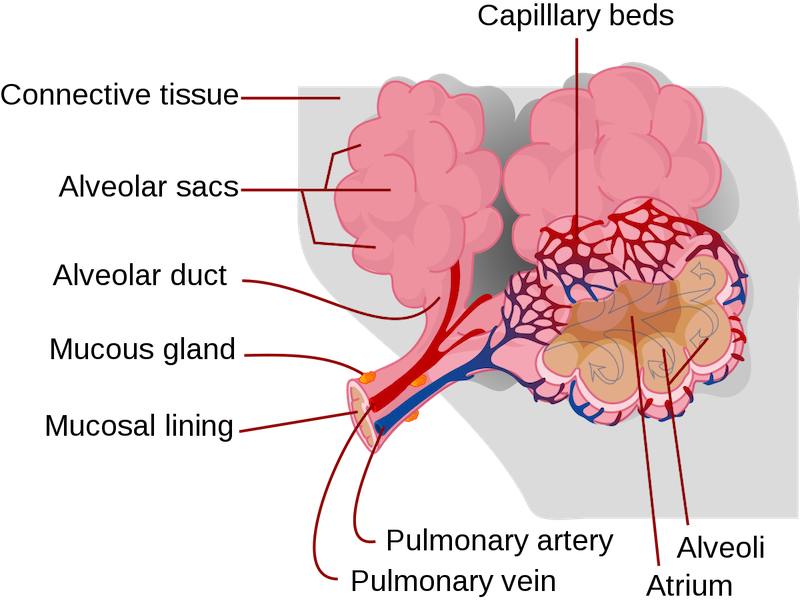 (Image Credit: Wikipedia)
(Image Credit: Wikipedia)
Sponsored Content:
Fraction of inspired oxygen (FiO2) is the molar or volumetric fraction of oxygen in the inhaled gas. FiO2 may be expressed as percentage or a decimals e.g. room air at sea level is 21% oxygen (0.21) and pure oxygen FiO2 = 100% (1.0).
The partial pressure of oxygen, (PaO2) is a measurement of oxygen partial pressure in arterial blood. The value reflects how well oxygen is able to move from the lungs to the blood, and it is often altered by severe illnesses. Normal PaO2 values = 80-100 mmHg. Hypoxemia is PaO2 < 50 mmHg.
Ratio of PaO2/FiO2: The ratio of the partial pressure of oxygen in arterial blood to the fraction of oxygen in inspired may be used as an indicator of hypoxemic respiratory failure. For example in healthy people, the ratio is between 300-500 mmHg. A ratio below 300 indicates that oxygen movement across the alveoli is diminished.
Ventilation: Moving air in and out of the lungs. Minute ventilation is calculated from the number of breaths per minute (respiratory rate RR) multiplied by the volume of air with each breath (tidal volume Vt). Changes in respiratory rate will change the level of carbon dioxide (CO2) in the blood, the faster the rate, the lower the CO2 level and vice versa. Oxygen delivery to the alveoli can be increased by increasing the inspired oxygen concentration.
Positive end expiratory pressure (PEEP): a pressure applied by the ventilator at the end of each breath to ensure that the alveoli remain open.
Flow: Speed in liters per minute at which the ventilator delivers breaths.
Continuous positive airway pressure (CPAP): Non invasive mask which fits tightly to the face and provides continuous pressure which in turn, prevents alveoli from closing. Also BiPAP: Bilevel positive airway pressure.
Acute respiratory failure (ARF): The most common organ failure observed in the ICU occurring with many concurrent diseases. The underlying problem is impaired gas exchange. ARF can be divided into two types:
- Oxygen failure – Hypoxemic respiratory failure (Type I) is characterized by an arterial oxygen tension (PaO2) lower than 60 mm Hg with a normal or low arterial carbon dioxide tension (PaCO2).
- Ventilation Failure: Hypercapnic respiratory failure (Type II) is diagnosed in patients without chronic lung disease when there is hypoxia and acute elevation of arterial PaCO2 >45 to 50 mm Hg and associated acidosis (pH <7.35).
Diagnostics for ARF include chest x ray, ABGs, and EKG (to rule out cardiac disease). Note: not everyone who has ARF goes on to develop ARDS.
Acute Respiratory Distress Syndrome (ARDS) is a condition that causes fluid to build up in the lung which then prevents oxygen from moving from the alveoli into the circulation. ARDS is an end-organ response of the lungs to syndrome of multisystem dysfunction or failure. The cause of ARDS is a non cardiac pulmonary edema due to an increase in permeability of the alveolar capillary membrane.
ARDS Definition (Berlin): The onset must be within one week of a clinical insult or new or worsening respiratory symptom. Chest xray must show bilateral opacities not fully explained by effusions (ground-glass appearance, lung collapse or nodules). The respiratory failure cannot be fully explained by cardiac failure or fluid overload.
Three levels of ARDS were identified based on the severity of hypoxemia:
- Mild ARDS (200 mmHg < PaO2/FiO2 < 300 mmHg) with CPAP or PEEP of at least 5 mmH20
- Moderate ARDS (100mmHg < PaO2/FiO2 < 200 mmHg) with CPAP or PEEP of at least 5 mmH20.
- Severe ARDS (PaO2/FiO2 < 100 mmHg) with CPAP or PEEP of at least 5 mmH20.
Causes of ARDS:
- Sepsis.
- Inhalation of harmful substances such as smoke or chemical fumes, inhaling (aspirating) vomit or near-drowning episodes.
- Viral or bacterial severe pneumonia usually affecting all five lobes of the lungs. Over 90% of the patients that die from COVID-19 die from ARDS. As the immune system attacks the coronavirus, inflammation occurs within the lungs causing fluid to build up in the alveoli and the person becomes starved of oxygen.
- Head, chest or other major injury.
- Pancreatitis (inflammation of the pancreas), massive blood transfusions and burns.
Pathophysiology Processes of ARDS: Include excessive alveolar-capillary membrane permeability, interstitial edema, diffuse alveolar injury, macrophage dysfunction, increased risk of infection.
The clinical presentation signs and symptoms may vary initially but later will correspond with the phase of pathophysiological response.
- Exudative Phase (72 hours after initial injury) where severe lung inflammation and edema occurs, capillary leakage increases and type 1 cells are destroyed. Terminal bronchioles become compressed and fluid leaks into the alveoli. The patient may become restless, RR will increase, dyspnea occurs, accessory muscles may be in use, oxygen levels will be normal and so may the x-ray.
- Fibroproliferative Phase – destruction of type II cells leads to loss of surfactant. Lungs become still and less oxygen is exchanged. Atelectasis occurs. Ventilation and perfusion are mismatched as the dead space increases (areas where there is no oxygen exchange). The patient becomes increasingly agitated, hypoxia gets worse and the patient works hard to breath. ABGs show decreased PaO2 and increased PaCO2 even with increased oxygen. Blood pH drops leading to respiratory acidosis. Lung sounds will be crackly and x ray will show infiltrates.
- Resolution occurs over weeks to months with increasing oxygenation and slowly clearing chest x ray. Lung function improves. Type II alveolar cells increase and restore surfactant.
In summary, Adult Respiratory Distress Syndrome is a form of respiratory failure characterized by acute lung inflammation and diffuse alveolar-capillary injury resulting in severe pulmonary edema. The lungs become wet and heavy, congested and stiff which in turn leads to severe hypoxemia and respiratory failure. Other complications include cardiac dysrhythmias, barotrauma, disseminated intravascular coagulation, congestive heart failure and renal failure. Understanding the physiology behind healthcare simulation can help all team members contribute to an ARDS simulation which in turn, helps healthcare practitioners promptly identify and treat ARDS.
Additional Reading: “NIH’s Explanation of Acute Respiratory Distress Syndrome“: Acute respiratory distress syndrome (ARDS) is a serious lung condition that causes low blood oxygen. People who develop ARDS are usually ill due to another disease or a major injury. In ARDS, fluid builds up inside the tiny air sacs of the lungs, and surfactant breaks down. Surfactant is a foamy substance that keeps the lungs fully expanded so that a person can breathe. These changes prevent the lungs from filling properly with air and moving enough oxygen into the bloodstream and throughout the body. The lung tissue may scar and become stiff. ARDS may develop over a few days, or it can get worse very quickly. The first symptom of ARDS is usually shortness of breath.
Other signs and symptoms of ARDS are low blood oxygen, rapid breathing, and clicking, bubbling, or rattling sounds in the lungs when breathing. ARDS can develop at any age. To diagnose ARDS, your doctor or your child’s doctor will do a physical exam, review the patient’s medical history, measure blood oxygen levels, and order a chest X-ray. Supplying oxygen is the main treatment for ARDS. Other treatments help make you more comfortable or aim to eliminate the cause of ARDS. Treatments for ARDS may help prevent serious or life-threatening complications, including organ damage or organ failure.
Read the Entire Physiology: The “Force” Behind Healthcare Simulation HealthySimulation.com Article Series:
- Part 1: Blood Pressure
- Part 2: Heart & Respiratory Rate
- Part 3: Pulse Oximetry
- Part 4: Diabetes
- Part 4B: Hypoglycemia & Excel Template for Simulated EHR
- Part 4C: Insulin
- Part 5: Sepsis
- Part 6A: Hypovolemia (Intro)
- Part 6B: Hypovolemia (Treatment & Simulation Tips)
- Part 7A: IV Fluids & Bags
- Part 7B: IV Pumps & Site Access
- Part 7C: PCA for Pain
- Part 8: ABGs
- Part 9: Sepsis Labs
- Part 10: Intro to Cardiac Rhythms
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!
Dr. Kim Baily, MSN, PhD, RN, CNE has had a passion for healthcare simulation since she pulled her first sim man out of the closet and into the light in 2002. She has been a full-time educator and director of nursing and was responsible for building and implementing two nursing simulation programs at El Camino College and Pasadena City College in Southern California. Dr. Baily is a member of both INACSL and SSH. She serves as a consultant for emerging clinical simulation programs and has previously chaired Southern California Simulation Collaborative, which supports healthcare professionals working in healthcare simulation in both hospitals and academic institutions throughout Southern California. Dr. Baily has taught a variety of nursing and medical simulation-related courses in a variety of forums, such as on-site simulation in healthcare debriefing workshops and online courses. Since retiring from full time teaching, she has written over 100 healthcare simulation educational articles for HealthySimulation.com while traveling around the country via her RV out of California.
Sponsored Content: