ASPiH 2021 Challenges Healthcare Simulation Professionals to Move Upstream, Facilitate Change
As healthcare simulation is constantly evolving, sharing the latest insights helps facilitate industry-wide advances. To accomplish this each year, the Association for Simulated Practice in Healthcare (ASPiH), a UK-based non-profit membership organization formed in 2010, hosts a clinical simulation conference and brings together the greater healthcare simulation community. This year’s conference, made virtual due to the coronavirus pandemic, featured the theme “Moving upstream — using clinical simulation to improve systems.” This article, written by HealthySimulation.com contributor Jeanne Carey, explains how this theme applies to healthcare simulation and shares pivotal moments from the ASPiH 2021 virtual conference.
The “River Story” anecdote used to reel in attendees to the ASPiH 2021 Virtual Conference was a fitting introduction to the opening keynote addresses. The story goes like this: Two friends are walking along a riverbank when they notice a child in the water, struggling to stay afloat. The two friends jump in and rescue the child. As soon as they have carried the child out of the water they notice another child in the river, also in difficulty.
While they are back in the water, they notice another child further upstream floating towards them. One of the friends then swims towards the shore and starts walking up along the riverbank. The person left in the water says: “Where are you going? There are more kids drifting down towards us.” To which the person walking away replies: “I’m going to see who’s throwing these kids in the water.” (ASPiH, 2021).
Sponsored Content:
This idea of looking upstream to prevent downstream problems is being considered by a multitude of industries, from legal aid and public health to artificial intelligence and self-driving cars. Most everyone can seemingly agree, preventing a problem is far superior to fixing one — and yet, moving in the direction of being proactive, instead of reactive, is quite challenging.
This requires consideration of other perspectives and acknowledgment that current conditions are less than ideal. And making your way upstream to identify the source(s) of the problem, takes a great deal of effort, especially if there is a swift current working against you.
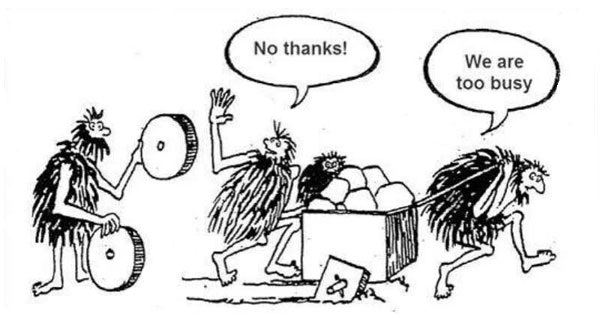
Michael Moneypenny, the current President of ASPiH, invited attendees to use the conference as an opportunity “to stop pushing the cart with square wheels” and take this time to step back and see if there is a better way to do things. He admitted that when he first started using healthcare simulation to train other anesthesiologists, he was all about the technical skills, “getting the right tube down the right hole”. Over time, he came to realize that these anesthesiologists were part of a team that needed to work within a system and there were many factors that affected the individual’s ability to safely perform this skill (ASPiH, 2021).
Sponsored Content:
Moving Upstream
At ASPiH 2021’s virtual conference, held from November 8 to November 10, there were nearly 400 delegates in attendance. The conference theme, “Moving Upstream: Using Simulation to Improve Systems”, permeated the sessions and encouraged participants to question their current focus in clinical simulation and where it should be. Much of the medical simulation being conducted in healthcare today is for the purpose of educating and training individuals.
ASPiH 2021 asked simulationists to consider whether using clinical simulation to make the system safer for the individuals to work in would be a more effective use of resources. Improving processes, procedures, guidelines, layout of spaces, and equipment may have wider and longer-lasting effects on healthcare delivery. Conference speakers did not suggest simulationists stop pulling people out of the river, i.e., training individuals, after all addressing the downstream problem is often a necessary, lifesaving intervention. They simply asked attendees to move upstream and think about using healthcare simulation in a different way.
Upstream Thinking – Working Better Together
Dr. Victoria Brazil, professor of emergency medicine and director of simulation at the Gold Coast Health Service, Bond University, delivered the opening keynote address, highlighting her work in translational simulation. This systems-based simulation aims at improving patient care and healthcare systems, through the detection of safety and performance issues, and the discovery of healthcare simulation-based solutions.
In translational simulation, the focus is on the purpose of the activity, irrespective of the location, modality, or content. Translational simulation activities may be diagnostic (determining what problems exist), interventional (providing solutions to problems), or a combination of the two (Nickson et al., 2021).
Healthcare teams face complex challenges while working within complex systems. Dr. Brazil noted good teamwork within healthcare is hard because of the complexity; there are so many highly trained individuals trying to work together. The current approaches to improving team performance, those emphasizing the behaviors of the team members, are not enough. As the healthcare system becomes more complex, training needs to focus on the interface of team members within the systems they work. Systems-based simulation can be used to explore work environments and close the gap between “work as imagined and work as done”.
Healthcare simulation should be considered as a strategy, rather than an event. This methodology can be used for much more than the education and training of individuals and teams. After all, healthcare teams are often ad hoc or swarm teams, highly trained individuals brought together to achieve common goals for the duration of the task but who lack the experience of training or working together as a team.
Dr. Brazil used the example of a 30-year-old victim of a motorcycle accident. The trauma team involved in the care of this patient may number as many as 70 members, amassed from a pool of more than 800. Training all the possible iterations of this team is not going to happen. But exploring the systems that this team must function in, can happen, and can make a difference in the outcomes of this patient.
Simulation for Organizational Learning, Bridging the Gap
Every system is perfectly designed to get the results it gets (Heath, 2020). To realize better results, change is necessary. Healthcare simulation can help organizations identify areas for improvement in processes, procedures, and design.
Michael Rosen, Associate Professor of Anesthesiology and Critical Care Medicine and Human Factors Psychologist at Johns Hopkins School of Medicine, built on Dr. Brazil’s presentation by examining the organizational and human factors that impact patient outcomes. Healthcare organizations use team-based work structures to achieve their goals. No one individual can provide all that a patient needs, nor can he or she protect the patient from all potential harms lurking within this increasingly complex system. Teams are more effective in tackling complex tasks than individuals, but the systems they operate within can make or break the team’s success.
Clinical simulation is proven as a powerful tool for building individual and team expertise in healthcare. However, it is becoming increasingly clear that the design of the social and technical systems can limit or enhance the effectiveness of the individuals and teams functioning within them. Too often, a divide exists between those working within the systems and those responsible for the design and development of healthcare organizations. Dr. Rosen believes healthcare simulation is a natural bridge between these groups.
Becoming Upstream Preventers Rather Than Downstream Problem Solvers
Healthcare simulation professionals could easily spend all their time downstream trying to save all children floating in the river. However, ASPiH 2021 asked attendees to move upstream and stop the children from falling into the river in the first place. Conference organizers crafted a schedule of engaging presentations demonstrating how healthcare simulation can be the driving force behind system improvement. Clinical simulation can support the transition of a complex healthcare system, from one comprised mostly of downstream problem solvers, to a high-performing system with upstream problem preventers.
Learn More About ASPiH
References:
Eliot, L. (2020, April 3). The venerable upstream parable helps in these trying times, and applies to the future of AI self-driving cars. Forbes. Retrieved November 9, 2021, from https://www.forbes.com/sites/lanceeliot/2020/04/03/the-venerable-upstream-parable-helps-in-these-trying-times-and-applies-to-the-future-of-ai-self-driving-cars/?sh=7f1b41880e9b.
Heath, D. (2020). Upstream: The quest to solve problems before they happen. Avid Reader Press.
Nickson, C. P., Petrosoniak, A., Barwick, S., & Brazil, V. (2021). Translational simulation: From description to action. Advances in Simulation, 6(1). https://doi.org/10.1186/s41077-021-00160-6.
Jeanne Carey is the Director of Simulation at Baylor University Louise Herrington School of Nursing in Dallas, Texas. She holds advanced certification as a simulation educator and has 10 years of experience in all aspects of simulation, including the development and implementation of new simulation-based learning activities, training of simulation facilitators, and recruitment and management of standardized patients. Carey and the LHSON Simulation Team created the Two-Heads-Are-Better-Than-One (2HeadsR>1) strategy for role assignment in simulation. She is active in several simulation organizations and currently serves as an INACSL Nurse Planner.
Sponsored Content: