Using Translational Simulation in Healthcare to Improve Patient Outcomes
In the past, the goals of outcomes of healthcare simulation focused simply on clinical skills or knowledge acquisition. More recently, some of the focus has shifted to teamwork behaviors and communication. Importantly, outcome measurements are available for all of the above domains. However, Clinical Simulation that involves a consideration for institutional culture, relationships between individuals and patient safety outcomes are not nearly as common possibly because these simulation scenarios are hard to design, involve multiple disciplines and have outcomes which are more difficult to measure. Here, Dr. Kim Baily PhD, MSN, RN, CNE, previous Simulation Coordinator for Los Angeles Harbor College and Director of Nursing for El Camino College, takes a closer look at Translational Simulation in Healthcare!
Connecting education, research and patient outcomes is difficult although translating research evidence to clinical practice is essential to safe, transparent, effective and efficient healthcare provision and meeting the expectations of patients, families and society. Research evidence is being produced at an increasing rate, however, change in clinical practice to reflect this evidence has lagged behind.
Dr. Victoria Brazil from Bond University and Gold Coast Health Australia, suggests that translational simulation can be used to link educational activities to patient level outcomes even though measurement outcomes may be harder to measure. Brazil suggests that medical simulation should focus on “not where but why”. “Descriptions of simulation type often use the device (e.g. high fidelity mannequin simulation) or place, e.g. in situ simulation (ISS), but these descriptors underplay the critical importance of outcomes from simulation, e.g. individual competence, team behaviors or patient level outcomes” (Brazil Advances in Simulation (2017) 2:20. DOI 10.1186/s41077-017-0052-3).
Sponsored Content:
Translational simulation encompasses the concept of Systems Integration defined by the Society for Simulation in Healthcare (SSH) as “those simulation programs which demonstrate consistent, planned collaborative, integrated and iterative application of simulation-based assessment and teaching activities with systems engineering and risk management principles to achieve excellent bedside clinical care, enhanced patient safety, and improved metrics across the healthcare system”.
Improving Patient Outcomes
Brazil used Berwick’s systems approach to improving care to create a framework for how healthcare simulation might be used to improve healthcare:
- What are we trying to accomplish? How much can be accomplished in one nursing simulation. Attempting to include too many objectives will likely lead to less being achieved.
- How will I know if a change leads to an improvement? How will the effect on a specific patient outcome be measured.
- What changes could we make that we think will result in improvement? Appropriately targeted, translational simulation offers a range of interventions for individual, team and system level improvement, ideally embedded within an integrated ‘translational science’ model.
Brazil suggests that translational simulation, education and training should be directed to a specific healthcare outcome target. Educators should not assume that just because simulation results in a learner with improved skills or increased knowledge that this will translate into better patient outcomes since complex, context-specific system issues are also involved. Translational simulation activities are likely to be most effective when explicitly integrated with an institutional quality improvement program (Braddock et al. The TRANSFORM Patient Safety Project: a microsystem approach to improving outcomes on inpatient units. J Gen Intern Med. 2015;30:425–33). Examples of simulation leading to improvement of patient outcomes include lowered central line infection rates and reduction in perinatal asphyxia.
Sponsored Content:
Translational science (TS) has been defined as a three step process from bench to bedside:
- T1 science: Basic laboratory discoveries in the biomedical sciences.
- T2 science: Evidence of T1 effectiveness provide “the right treatment for the right patient in the right way at the right time”. Once these standards have been identified they should be developed into practice guidelines for patients, clinicians, and policy makers.
- T3 science: Consideration of health-care delivery, community engagement, and preventive services that produce measurable improvements in the health of individuals and society.
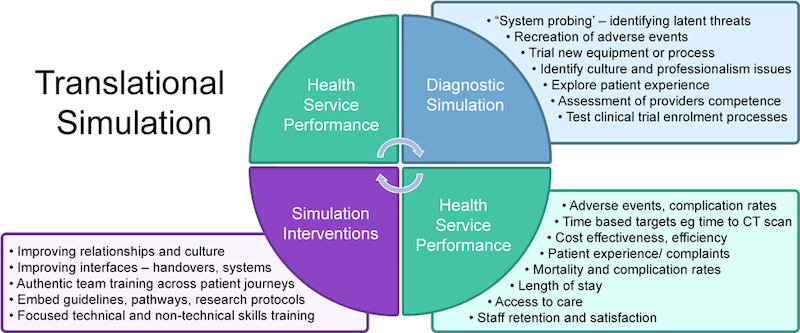
Translational Simulation can be divided into two main categories:
- Diagnostic simulation which includes system probing, recreation of adverse events, trailing new equipment/processes, identifying cultural and professional issues, exploring patient experiences and assessment of provider competence.
- Simulation interventions which includes improving relationships and culture, improving interfaces such as handovers, authentic team training across entire patient journeys, embedded guidelines, pathways, research protocols, and focused technical and non-technical skills training.
- Both categories of translational simulation are related to health service performance such as adverse events, complication rates, time based targets, cost effectiveness/efficiency, patient experience/efficiency, mortality, length of stay, access to care, and staff satisfaction and retention.
Relatively few references are found in the literature related to relational aspects of care including culture even though even though these are likely to impact patient outcomes. Brazil notes that “educational, clinical, quality, and safety goals can only be achieved by thematic, sustained, and cumulative research programs, not isolated studies”. Brazil notes that national funding priorities should be support translational education research. In the United States, the National Institutes of Health (NIH) and the Institute of Medicine translational science policies focus on biomedical research, education of biomedical scientists, and conventional treatment options but do not address the value of a skilled health professions workforce and the importance of rigorous clinical education for the delivery of effective health care.
Simulation-based medical education (SBME) can contribute to translational science when the outcome of the simulation is related not only to the immediate outcome of the learning experience (simulation) but more importantly to outcomes related to better healthcare delivery and patient outcomes. Translational simulation first plays a role in diagnosing safety issues and then by creating simulation-based interventions to address the safety issues.
Read the Full Research Article: “Improving the relational aspects of trauma care through translational simulation“
Have a story to share with the global healthcare simulation community? Submit your simulation news and resources here!
Dr. Kim Baily, MSN, PhD, RN, CNE has had a passion for healthcare simulation since she pulled her first sim man out of the closet and into the light in 2002. She has been a full-time educator and director of nursing and was responsible for building and implementing two nursing simulation programs at El Camino College and Pasadena City College in Southern California. Dr. Baily is a member of both INACSL and SSH. She serves as a consultant for emerging clinical simulation programs and has previously chaired Southern California Simulation Collaborative, which supports healthcare professionals working in healthcare simulation in both hospitals and academic institutions throughout Southern California. Dr. Baily has taught a variety of nursing and medical simulation-related courses in a variety of forums, such as on-site simulation in healthcare debriefing workshops and online courses. Since retiring from full time teaching, she has written over 100 healthcare simulation educational articles for HealthySimulation.com while traveling around the country via her RV out of California.
Sponsored Content: