New Research Suggests CPR Manikins Find Only 2% of Learners Competent
While cardiopulmonary resuscitation is known to significantly increase the rate of patient survival following cardiac arrest, CPR only works when applied correctly. So what happens when learners learn incorrectly during clinical simulation? While we might think that human instructors assess better than resuscitation simulators, new research shockingly suggests that CPR manikins find only 2% of learners are competent, compared to 90% of instructors who scored adequate performance! Here, Dr. Kim Baily PhD, MSN, RN, CNE, previous Simulation Coordinator for Los Angeles Harbor College and Director of Nursing for El Camino College covers recent a study by Hansen et al. which shockingly reveals that certified basic life support (BLS) instructors failed to identify resuscitation skills accurately when compared to human patient simulators.
Successful resuscitation outcomes are dependent not only on quick interventions but also on the skill of the people conducting the interventions. Thorough basic life support (BLS) training and adequate regular practice contribute to the skill of the rescuers. A recent study by Hansen et al., revealed that certified basic life support (BLS) instructors failed to identify resuscitation skills accurately. (Hansen, C., Bang, C., Staerk, M., Krogh. K., & Lofgren, B. Certified Basic Life Support Instructors Identify Improper Cardiopulmonary Resuscitation Skills Poorly. Simul Healthc 2019; 14:281-286).
The 2015 European Resuscitation Council (ERC) Guidelines for basic adult life support recommend chest compressions with a depth of 50 to 60 mm, a rate of 100-120 per min and rescue breaths with a tidal volume of 500-600 mL. (American Heart Association has similar recommendations, 2 – 2.4 inches for chest compressions, rate 100-120). This study involved peer instructors (senior medical students) who had completed a 2-day instructor course and who had more than 3 years of experience as instructors. Student training consisted of 4 hours of either instructor led demonstrations or formal lecture or a combination of both, followed by hands on experience.
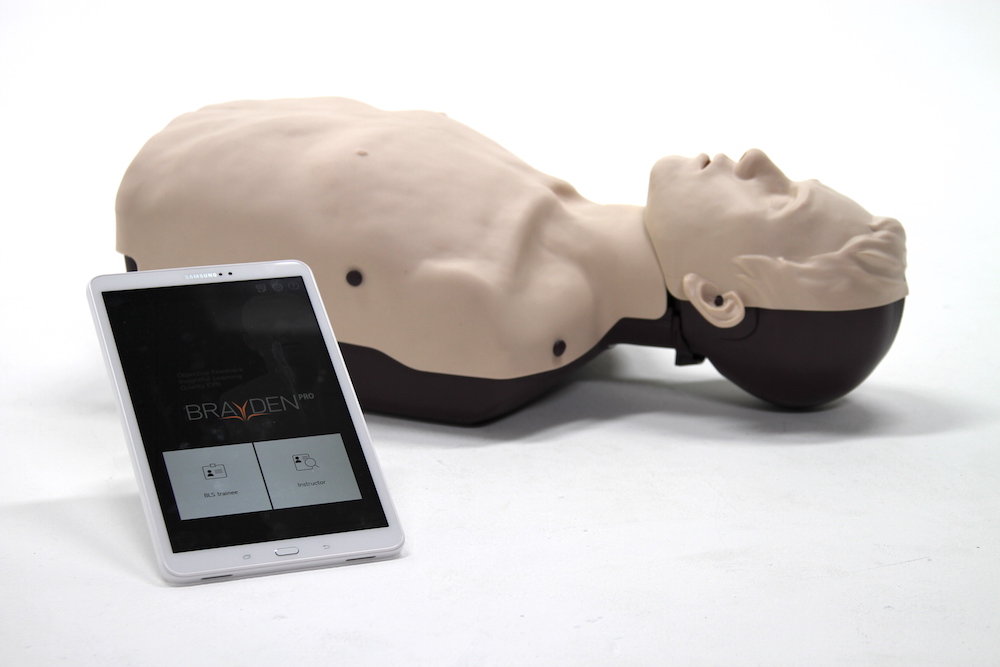
Sponsored Content:
Following completion of the course, all students were assessed using a resuscitation manikin. Instructors assessed all steps of the BLS algorithm. Instructors did not assess any of the students they had trained during the course. Each learner was assessed by two instructors who reached a consensus about a student’s particular performance. The instructors did not receive any information from the manikins.
Ninety CPR assessments were evaluated by 16 instructor pairs. (28 instructors, four of them twice). The mean age of the students was 22 years and 62% were female. The instructor assessments were compared against data received from the manikins for each cycle of CPR for chest compressions (overall, depth and rate) and rescue breaths.
Instructors assessed 81 (90%) of learners as competent in combined chest compressions and rescue breaths however data from the CPR manikins indicated only 2% were competent. Instructors failed one student for improper chest compressions even though manikin data assessed the student as satisfactory. Instructor assessment of rescue breaths alone matched the manikin data (7% learners), however, 80 (89%) improper rescue breaths were not identified by the instructors.
This result indicates that instructors using “visible chest rise” as an indicator of satisfactory rescue breaths is not accurate since many students did not achieve an adequate tidal volume (500-600 mL). These findings could be explained by lower volumes than those recommended for adequate CPR resulting in a manikin chest rise or the manikin reports lower tidal volumes compared with what is performed. Different results may have been found with other manikins than those used in this study. Regardless, manikin manufactures should ensure that their products accurately display equivalent volumes that will match CPR guidelines.
Sponsored Content:
Relatively few learners performed correct chest compressions related to depth and rate with rate being more accurate than depth. Interestingly, a difference was found between males and females with males tending to perform chest compressions that were too deep and females chest compressions that were too shallow. According to this article, other studies have found that exertion is greater in females than males but this difference disappeared when BMI, age and physical fitness were corrected for. The authors note that taller practitioners were more likely to perform correct chest compressions.
The above data is significant since certified BLS instructors were able to assess learners with high sensitivity but with very limited specificity. The data from CPR manikins appears to be a better indicator of learner performance and therefore should be included whenever possible. Without such manikin generated data to enhance CPR education, CPR performance in real life may be compromised. This ultimately may affect survival in actual CPR.
The American Heart Association recommends the use of objective performance data to enhance both BLS and ACLS education and outcomes. This adds additional cost to training and the need for periodic validation of equipment. Audiovisual feedback during training could add to training and as well as during actual resuscitation attempts in patients.
Read the Entire CPR Manikin Performance Article Here!
Dr. Kim Baily, MSN, PhD, RN, CNE has had a passion for healthcare simulation since she pulled her first sim man out of the closet and into the light in 2002. She has been a full-time educator and director of nursing and was responsible for building and implementing two nursing simulation programs at El Camino College and Pasadena City College in Southern California. Dr. Baily is a member of both INACSL and SSH. She serves as a consultant for emerging clinical simulation programs and has previously chaired Southern California Simulation Collaborative, which supports healthcare professionals working in healthcare simulation in both hospitals and academic institutions throughout Southern California. Dr. Baily has taught a variety of nursing and medical simulation-related courses in a variety of forums, such as on-site simulation in healthcare debriefing workshops and online courses. Since retiring from full time teaching, she has written over 100 healthcare simulation educational articles for HealthySimulation.com while traveling around the country via her RV out of California.
Sponsored Content: