When Simulation Goes Too Far… Dangers Become Real
When I first started as a simulation technician in 2008 I was warned by my clinical educator Brad Brown of a rumor that some nursing students had been in a simulation lab playing around with an AED thinking it was also “simulated”. The rumor goes that the AED was not a training model but a fully functioning device which administered a shock to one of the students, killing them in the simulation lab. True or not, Since then I have always confirmed the range of functionality in AED’s in all of the simulation programs I’ve worked in.
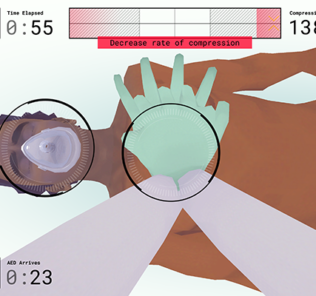
One of the primary reasons to utilize simulation is the dramatic increase in safety of all potential participants. In construction CAT simulators can help reduce the likelihood of vehicle accidents to driver or nearby workers. In Aviation, flight simulators reduce the physical risks to new pilots, trainers, passengers and those on the ground. In healthcare, simulation reduces the risk of harm to a patient while learning a new procedure. But when simulation is not treated with the greatest of respect, there can be lethal consequences.
Sponsored Content:
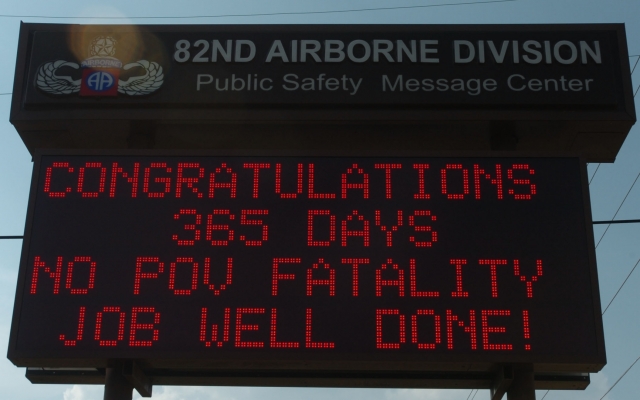
I was shocked to learn about the dangers of simulated military training from friend Mike Fischer who served as a Para Trooper in the US Army 82nd Airborne Division. While stationed at Fort Bragg leadership reminded newly stationed Para Troopers like Mike that the goal was to go 82 days without a fatality — a goal that had never been achieved before (and would remain so until over a decade later). Jumping out of planes at minimum safety elevations with live ammunition is certainly a recipe for fatal error.
While training at El Camino Fire Academy, Instructors waited until the class had proven its ability to work as a team and respect the live-fire spaces we were entering before ever actually letting us see real fire. Fire, will predictable, is never entirely controllable — and indeed there was at least one day when the fire became unruly and training plans were instantly abandoned by our instructors in favor of “immediately extinguishing that flame”. Clipboards were thrown that day.
Just last week in Sydney, a bomb training device had been brought on board a Passenger Ferry without previous administrative warning.
“A bomb scare on a ferry that caused major disruptions in downtown Sydney was a training exercise gone wrong, an official said Friday. The transport hub of Circular Quay, between the iconic Sydney Opera House and Harbour Bridge, was shut for two hours Thursday afternoon after the crew of a moored ferry found a suspicious package.
Sponsored Content:
Bomb squad police were called to examine the package, which was described by Australian Broadcasting Corp. as two bottles containing liquid and nails with protruding wires. Steffen Faurby, chief executive of Harbour City Ferries, which operate the Sydney fleet, on Friday described the package as “a training device, which was not recognized as a typical training device by staff.” Read the full EMS World article here.
Arming police and bomb squads and injecting them into what appears to be life threatening situations has the potential to bring unnecessary injuries to many.
While thankfully the simulated training we as healthcare professionals (outside of the Fire Services) is less personally dangerous — the potential for damage to ourselves or others still remains.
Simulation Materials Outside the Lab Cause Real Life Patient Injuries
Last month, simulated IV solutions bags were used on actual patients — causing illness to at least 40 patients across a multitude of states.
“Back on December 30th, FDA alerted health professionals about a patient who became ill after receiving an IV solution meant for training purposes only. Educators often utilize training products for simulations with students and want these items to look like the real solutions. However, there have been serious adverse events associated with misuse. These solutions aren’t sterile and should never be used in humans or animals.
Since the initial alert we learned of additional patients who received these solutions since the earlier alert and late Wednesday evening FDA published a statement saying that over 40 patients have actually received these solutions, many suffering adverse events, including fever, chills, tremors and headache. Some patients were hospitalized, and there is one death associated with the use of these products although it’s not known if this death is directly related to the use of the product. Adverse events have been reported in seven states: Florida, Georgia, Idaho, Louisiana, North Carolina, New York, and Colorado.” Read the full article on Philly.com
The manufacturer of the solutions noted in the FDA alert, said it has recalled current products, including IV bags filled with sterile distilled water. I don’t place much blame the manufacturer — these products are designed to mimic reality as closely as possible in-order to maximize the fidelity of our training solutions. But just as an AED can be too real in a simulation lab, so too can simulation materials outside of the lab. How did these products escape their lab? Considering the rapid adoption of simulation technologies in healthcare facilities around the world, the potential for this oversight is quite large in our domain.
So many times I have seen simulation programs have to funnel their purchases through the same purchasing departments and processes as other normal supplies — and I have never agreed with that policy. Simulation IS special, and simulation supplies should be treated as such.
Strategies For Minimizing Patient Risk:
- Convince leadership to have simulated supplies be shipped directly to the simulation labs and skip normal medical supplies processing.
- Actually keep track of your simulation supplies. A box of sixteen simulated IV bags should be counted and properly managed through a single individual responsible for those items.
- Keep simulated carts separate from main carts with a lock that will NOT work without a simulation-specific staff member present. Simluated materials should never be mixed into patient care carts. Instead, another cart should be purchased that can contain whatever you want — but it is clearly labeled as a simulation only cart, locked and stored only in simulation specific areas
- Lock simulation specific areas if possible. Unless you are in-situ, simulation areas should be off limits. This not only reduces risks of supplies walking away, but physical damage or loss of expensive simulation equipment as well.
Perhaps Manufacturer’s need one clear label that demonstrates product is NOT FOR PATIENT USE. The article above argues “patient simulation” is too close to “Patient Situation”. Whereas NOT FOR PATIENT USE in red or orange is hard to miss. The article above suggests the manufacturer is already working on such indicators to help reduce future errors.
What Does Your Sim Lab Do?
What does you simulation program do to minimize risks of simulated medications or other simulated tools being used on actual patients?
Join the HealthySim Medical Simulation LinkedIn Discussion Group and let your community know!
Lance Baily, BA, EMT-B, is the Founder / CEO of HealthySimulation.com, which he started in 2010 while serving as the Director of the Nevada System of Higher Education’s Clinical Simulation Center of Las Vegas. Lance also founded SimGHOSTS.org, the world’s only non-profit organization dedicated to supporting professionals operating healthcare simulation technologies. His co-edited Book: “Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice” is cited as a key source for professional certification in the industry. Lance’s background also includes serving as a Simulation Technology Specialist for the LA Community College District, EMS fire fighting, Hollywood movie production, rescue diving, and global travel. He and his wife live with their two brilliant daughters and one crazy dachshund in Las Vegas, Nevada.
Sponsored Content: