Serious Games
A “serious game,” also known as an applied game, is a computer-based program that is designed for both entertainment and learning purposes, by simulating real-world scenarios. These applied games are often applicable across healthcare simulation education and training, with the learning tools able to accurately convey how a procedure or skill is meant to be performed in the field. By combining elements of entertainment with healthcare simulation, learners are able to master these skills in an environment that is engaging, is risk-free and promotes patient safety. Those interested in this topic should certainly check out the Serious Play Conference held annually!
Research has proven that video games improve performance of surgeons, and that they are a practical method for healthcare simulation training. They also allow learners to make their own decisions and begin to understand what is happening at each point during a serious game’s progression. As such, serious games enhance healthcare simulation training benefits by combining academic lessons with repetitive practice. Therefore, applied games help generate learning outcomes that increase content retention and comprehension, leading to long-term success across clinical settings. As decision-making processes are reinforced, learners are able to go on to become confident professionals and practitioners.
Serious games can further help learners to strengthen their problem-solving skills, adding to their overall professional development. These games are capable of being adapted to meet a variety of healthcare simulation training needs, from diagnosis to surgery. Applied games are helping to train learners in a new and engaging way. In addition, they can generally be played at any time and from anywhere remotely. This real-time cognitive game-based medical simulation education allows healthcare learners to complete coursework on their own time and at their own pace.
Sponsored Content:
Other benefits of serious games and gamified learning environments are that they are easily accessible, approachable and enjoyable. Through the deployment of textual, auditory and visual cues, serious games improve comprehension but are not bound by in-classroom restrictions. This creates a scenario where cognitive rewards are met with dynamic feedback. Each healthcare simulation debriefing is integral for any serious game play to yield optimal training benefits.
Serious game technologies can be also useful for training patients on topics like how to maintain health habits. For example, healthcare administrators can recommend serious game play for diabetes patients who need to learn better health management strategies. Applied games can help train patients on rehabilitation procedures and techniques as well.
The establishment of game-based problem-solving parameters within non-game contexts can continue to have a vast impact on medical simulation training as the field shifts to more remote and virtual learning alternatives. As developers and educators continue to employ this technology to educate learners, the training is sure to become even more realistic, comprehensive and effective.
Medical board games, critical thinking games for nursing students, and healthcare board games in general are all examples of serious games that offer unique learning opportunities for educational, training, and patient safety programs utilizing healthcare simulation methodologies to improve outcomes. From the ER to disease infection control, and from medical terminology to neonatal resuscitation, here is a comprehensive list of some of the best board games for healthcare, including some key research highlights which demonstrate educational success with the playful medium.
Sponsored Content:
An event held to explore the use of game-based learning, the Serious Play Conference is a leadership conference that offers a full track of sessions on every major market for the use of serious games and simulations in training or education as well as a full track on instructional/game design. During this conference, speakers and professionals can share their experience and work together to shape the future of training and education in the corporation, classroom, healthcare institution, government, military and many other industries. They also offer tips on how to move game-based education programs ahead. Founded in 2009 by Sue Bohle, the Serious Play Conference has become a place to keep current on the rapid changes and evolution of serious games.
Examples of Healthcare Simulation Serious Games
Developed by Education Management Solutions, SimPHARM is a virtual and clinical pharmacology healthcare simulation solution for learners and interprofessional education teams. The applied game is a web-based, virtual patient care training platform that creates a realistic clinical experience, through participation within a cross-functional medical training center or remote learning locations.
This serious game is built on mathematical models of the physiology of body systems that simulate real-life reactions to diseases and drugs. SimPHARM’s engine is built by leveraging the most up-to-date drug lists, categories, formulations, side effects and interactions, and acts in accordance with pharmacokinetic and pharmacodynamic principles.
Using SimPHARM, learners can experience the consequences of their therapeutic decisions. The healthcare simulation technology operates on a dynamic learning algorithm, by which every learner and team who run a case may experience a different outcome. SimPHARM’s clinical pharmacology-based simulation software is an ideal training solution for both undergraduate- and graduate-level education programs.
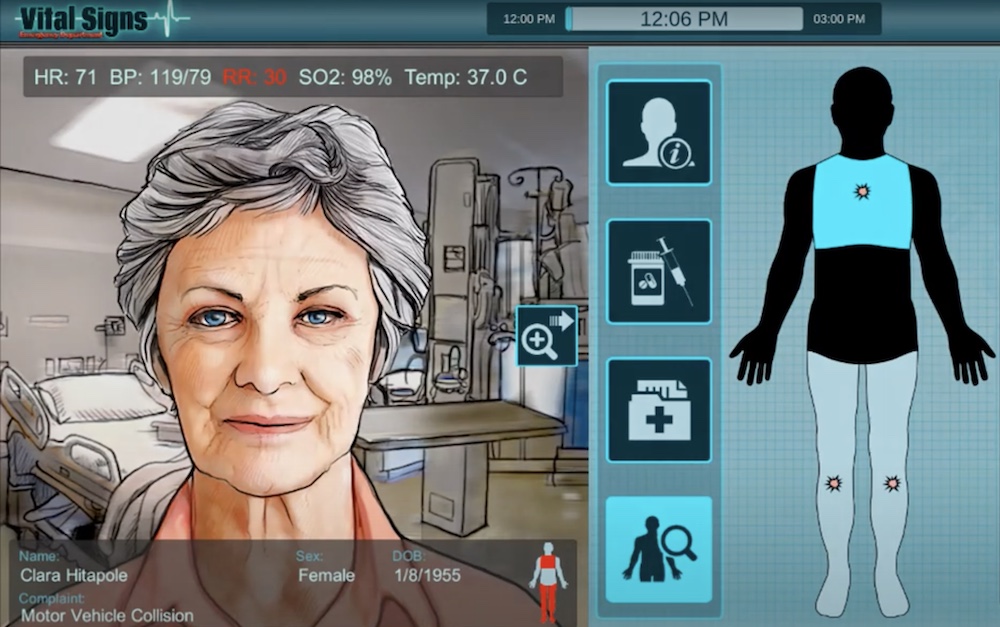
BreakAway Games, a video game developer based in Hunt Valley, Maryland, has also created a number of healthcare simulation serious games to help train learners. One of the applied games, Vital Signs: ED, allows the learner to take on the role of a physician working in an emergency department. The serious game recreates the stress and confusion of the ED, as the learner adapts to handle difficult trauma cases while the exam rooms fill up quickly with patients needing triage. With a short period of time to act, distractions, phone calls, disruptions and paperwork requirements, learners must make tough clinical decisions while pressure builds.
Touch Surgery is another serious game used to train surgeons and, as a result, save lives by leveraging the power of AI, data and visualization. The Touch Surgery interactive surgical simulator provides a realistic guide to surgical procedures; allowing medical simulation trainees to learn procedures, test their knowledge and rehearse for surgery. The app has over three million global users and provides secure, seamless access to surgical videos and data. This applied game application features the DS1 Computer, the first surgical simulation video recorder equipped with real-time AI, which automatically redacts sensitive frames in surgical videos.
“The eSMART-HD program is designed to empower people from medically and socially disadvantaged groups to more effectively self-manage their chronic illnesses, including negotiating for what they want and need,” Clochesy said. “The system helps people interact with their healthcare provider as realistically as possible. Participants were amazed at how much they learned during this virtual experience, and how real the entire process was.”
Grendel Games, in collaboration with domain experts, develops healthcare simulation serious games that can yield behavioral change, as well. The University Medical Center Groningen (UMCG) has used the company’s serious game, Underground, to train surgeons on the necessary motor skills and to meet necessary training hours.
“We wanted a game that would challenge trainee surgeons and encourage them to complete the necessary amount of training hours. We involved an education specialist who supported us with the teaching elements of the game. The Grendel Games team came up with a wonderful idea,” Henk ten Cate Hoedemaker, a surgeon and the mastermind behind the Underground serious game, said. Learn more about serious games by reading the articles below.
Serious Games Simulation Education Latest News

A Guide to Enhancing Healthcare Simulation Through Gamification

Global Healthcare Simulation News Update January 2024

Game Industry Charity, Child’s Play, Helps Children Play Games, Feel Better

Newest Clinical Simulation Research From Around the World

Top Healthcare Simulation Serious Games to Engage Clinical Learners

Latest Clinical Simulation News From Around the World | November 2021

Virteasy Dental Announces First Next-Gen Haptic Dental Simulator Built On Unreal Engine
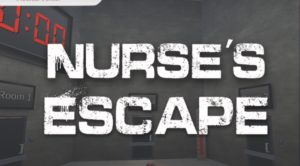
The Future of Educational Escape Rooms for Nurses
Sponsored Content: