Global State of Patient Safety: Annual Review
One of the major reasons for healthcare simulation is to improve patient safety and outcomes. Clinical simulation has been linked to improved patient safety and patient outcomes through deliberate practice and application of knowledge in a safe environment to learners for mistakes without potential harm to a patient. The Institute of Global Health Innovation at Imperial College London, commissioned by Patient Safety Watch, presents the analysis of the Global State of Patient Safety 2023. This HealthySimulation.com article will highlight the results of the Global State of Patient Safety in 2023.
Global State of Patient Safety 2023 Recap
According to the World Health Organization (WHO), Patient Safety “is the absence of preventable harm to a patient during the process of health care and reduction of risk of unnecessary harm associated with health care to an acceptable minimum.” Common healthcare errors include patients receiving the wrong medications, contracting hospital-acquired infections, having the wrong body part removed during surgery, receiving an incorrect diagnosis, or having a missed diagnosis or treatment.
Sponsored Content:
The patient safety country ranking compares the performance of OECD countries across four well-established patient safety indicators, following the methodology used by the Commonwealth Fund.The ranking also highlights the variation that exists across comparable countries. Using only the four selected metrics, the UK could have had 17,356 fewer deaths annually if the national healthcare systems had performed at the level of the top decile of Organisation for Economic Co-operation and Development (OECD) countries.
Broken down by indicator, this would have meant 15,773 fewer deaths classified as “treatable mortality” (where the cause of death can be mainly avoided through timely and effective health care interventions) per year, 776 fewer deaths due to neonatal disorders per year, 27 fewer maternal deaths per year and 780 fewer deaths due to adverse effects of medical treatment per year.
An important limitation of this ranking is that the four indicators included only represent a narrow aspect of health system performance, and do not consider the wider quality of life effects or long-term disability caused by unsafe care. More comprehensive, consistently collected, and regularly shared data would significantly increase the opportunity for cross-country comparisons and shared learning.
World Health Organization (WHO) on Patient Safety
Sponsored Content:
WHO published an interim report in April 2023, compiled of responses from 102 countries across all six regions. Progress against achieving the core indicators from the WHO GPSAP was measured:
- 27% of countries have developed a national patient safety action plan or equivalent
- 36% of countries have implemented a system for reporting of never events
- 18% of countries have signed up for implementation of the WHO Health Worker Safety Charter
- 31% of countries have established national targets on reducing healthcare-associated infection rates
- 13% of countries have a patient representative on the governing board (or an equivalent mechanism in 60% or more hospitals)
Patient Safety and Clinical Simulation
The role of healthcare simulation in improving patient safety expands every year however, persuading hospital and clinic administrators to increase funding for simulation may be challenging. Simulation in Healthcare helps create High-Reliability Organizations (HROs): HROs are organizations that have the potential for catastrophic failure yet engage in nearly error-free performance. The healthcare industry differs considerably from HROs, such as the airline industry, because of the variation in healthcare settings, the focus in healthcare on patients rather than machines, and the fact that failures occur to individuals rather than mass casualties. Extensive investigation and publicity follow major airline crashes, whereas individual adverse patient events do not receive the same attention.
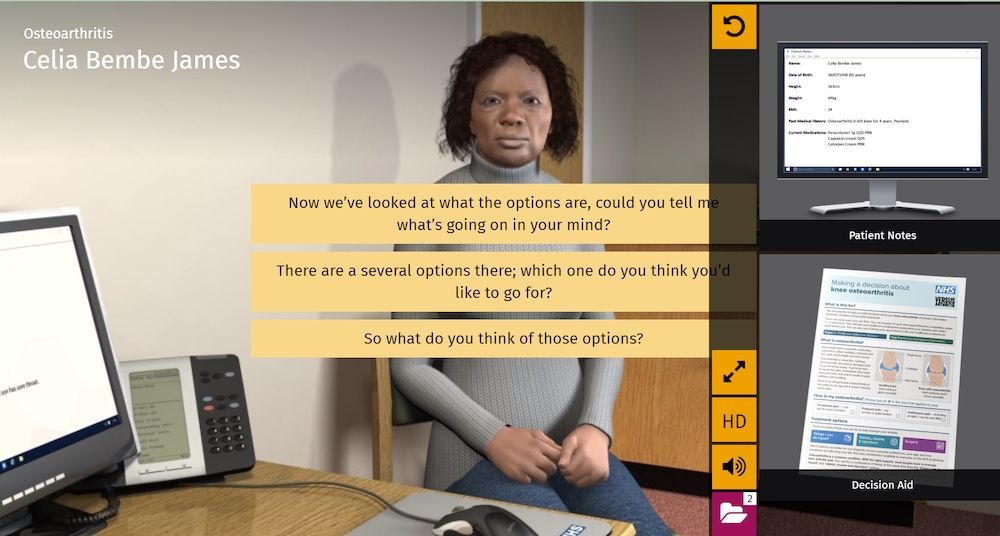
Healthcare simulation can help create a safety culture. Simulation can help create a proactive environment that is blame-free. Simulation training may be offered to individuals, teams, and larger units and scenarios can be created that match clinical situations that providers find the most worrisome. Simulation can be used to identify situations that have the potential to cause harm before they occur in actual practice. Educators know that simulation can produce moments of clarity for learners that will change their future practice for the better.
Simulation can be used to test and improve processes and procedures. The use of standardization operating procedures (SOPs) based on evidence-based practice throughout an institution prevents variability and reduces error. In addition, nursing simulation promotes flexible responses where every member of a team is empowered to speak up if they have a concern.
Case Studies
The case studies showcase excellence in safety measurement and improvement from the patient, family and carer perspective. These insights from nine leading patient safety experts and practitioners provide optimism on how deficiencies in patient safety data can be addressed. The challenge remains in how to foster the effective adoption of these approaches and interventions globally.
- Case Study 1: Involving Patients in Safety Investigations
- Case Study 2: Restoration and Healing from Harm
- Case Study 3: Safety Measurement and Monitoring Framework
- Case Study 4: Situational Awareness for Everyone (S.A.N.E.)
- Case Study 5: Family-Activated Medical Emergency Teams
- Case Study 6: No-Fault Maternity Compensation Schemes
- Case Study 7: Addressing Racial Disparities in Maternal Morbidity
- Case Study 8: Patient Measure of Safety
- Case Study 9: Partners at Care Transitions Measures
View the LEARN CE/CME Platform Webinar Saving Lives Systematically: Medical Simulation as a Patient Safety Tool in Healthcare to learn more!
Recommendations from The Institute of Global Health Innovation at Imperial College London
Based on the findings, three recommendations have been suggested to improve the measurement of patient safety:
- Assessment: A more balanced and comprehensive set of global patient safety indicators is required to address the data gaps identified in this report, and to ensure comparable data is available for all countries. Consensus is required on the minimum set of indicators that all countries should report on.
- Adoption: A global repository of safety measurement and improvement interventions should be developed and made freely available to frontline teams of practitioners and researchers across the world.
- Activation: To ensure the faithful adoption of interventions, patients, families, and carers must be given the agency to become active and equal partners in the delivery of safe care.
Learn More About Using Clinical Simulation to Improve Patient Safety!
Teresa Gore, PhD, DNP, APRN, FNP-BC, CHSE-A, FSSH, FAAN – Dr. Gore has experience in educating future nurses in the undergraduate and graduate nursing programs. Dr. Gore has a PhD in Adult Education, a DNP as a family nurse practitioner, and a certificate in Simulation Education. Dr. Gore is an innovative, compassionate educator and an expert in the field of healthcare simulation. In 2007l Teresa started her journey in healthcare simulation. She is involved in INACSL and SSH. She is a Past-President of INACSL and is a Certified Healthcare Simulation Educator Advanced (CHSE-A). In 2018, she was inducted as a Fellow in the American Academy of Nursing (FAAN). In 2021, she was inducted as a Fellow in the Society of Simulation in Healthcare Academy (FSSH) and selected as a Visionary Leader University of Alabama at Birmingham School of Nursing Alumni. During her career, Dr. Gore has led in the development and integration of simulation into all undergraduate clinical courses and started an OSCE program for APRN students. Her research interests and scholarly work focus on simulation, online course development and faculty development. She has numerous invited presentations nationally and internationally on simulation topics.
Sponsored Content: