Latest Clinical Simulation News Updates From Around the World: September 2019
A busy month for Clinical Simulation news updates from around the world — today we take a look at the latest updates showcasing the continued growth of our community and its work. From the latest medical simulation center to new vendor partnerships, media highlights, and research to new innovations in VR training and temporary tattoos for assisting medical training, here are some of the key updates from around the world of medical simulation:
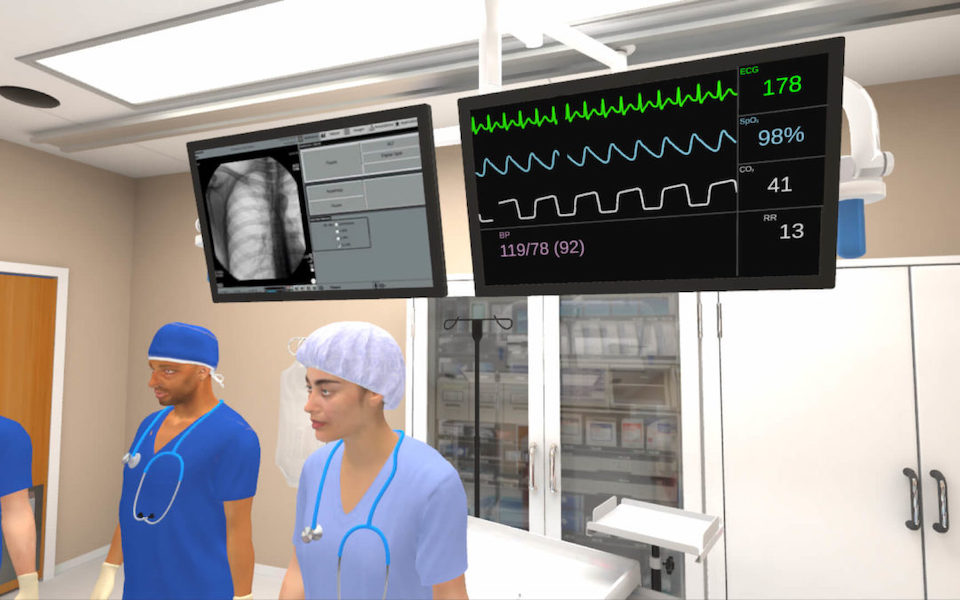
Mount Sinai HELPS Center Study Finds Virtual Reality ACLS Simulation Training Effective for Assessing ACLS Competency: The study found that VR simulation was predictive of clinicians’ overall performance in high-fidelity mannequin-based simulation and was 83% more cost effective. There was no statistically significant difference in assessing clinicians’ decision-making capabilities between VR and high-fidelity mannequin-based simulation. Additionally, the rank order of the clinicians’ performance in VR correlated with their rank-order in high-fidelity simulation, indicating that VR can predict how clinicians will perform in real-life scenarios. This is because high-fidelity mannequin-based simulation has previously proven to be an effective surrogate for real life encounters in the resuscitation domain.
Smith+Nephew, the global medical technology business, announces a collaboration with VirtaMed to provide surgical simulation training as part of their Training & Education portfolio for advanced surgical devices: “We have realized the value in simulation training as a meaningful part of the educational pathway and I am excited to bring this new method of training into our professional education activities,” stated María Jesús Barrenechea, Senior Vice President, Global Medical Education and Societies. “VirtaMed is clearly the most sophisticated simulation solution provider and is unique in their ability to adapt our devices for simulation.” VirtaMed will work together with senior experts from Smith+Nephew to identify the key learning objectives associated with each arthroscopic surgical technique and incorporate them into new simulation modules, combining anatomically correct models with photorealistic virtual reality simulation. These modules will be available for select VirtaMed customers who already own an ArthroS™ and of course as part of Smith+Nephew’s ArthroS global simulator fleet.
Sponsored Content:
Life and death inside the simulation: Future UT docs learn how to save lives before they have to: Put on for about two dozen Collierville chamber members, the event included a tour of UTHSC’s state-of-the-art Center for Healthcare Improvement and Patient Simulation (CHIPS), which has specialized simulation training equipment. See the slideshow at the top of the page for a virtual tour of the CHIPS facility That medical training equipment includes child and adult mannequins that mimic breath sounds, eye movements, and other lifelike motions necessary for training. Those mannequins can cost thousands of dollars, some even running from $60,000 up to $240,000. Other high-tech equipment at CHIPS includes a 3D virtual dissection board for anatomy and physiology education and simulators for minimally invasive surgery and for performing ultrasounds. For training purposes, all of the exam rooms, hallways, and even the elevators — medical care may need to be administered in an elevator, too — are equipped with video and sound monitoring.
Quinnipiac University medical school highlights prominent role of simulation: “When we go through the clinical scenario, we’ll have one person who is like the patient’s family member, one of the students will be the nurse, another will be the doctor,” said nursing student Alicia Ricci. “We all play different roles so we know what to do and what to expect in a scenario.” According to Rogers, manikins and simulation in medicine became popularized in the early 2000s. “At the time it was really nursing that was using the manikins,” she said. “Now it’s really evolved, over these past ten years especially, to start including different professions.”
Upstate Medical University on Thursday formally opened a new $11 million teaching center that will simulate real-time responses to medical emergencies: “The Upstate Simulation Center exemplifies our mission and vision to improve the health of our communities through education, biomedical research and health care and to create a healthier world for all,” Dr. Mantosh Dewan, interim president of Upstate Medical University, said in Upstate’s news release. “This special space provides Upstate with the ability to enhance the training of our students and our region’s health care professionals by addressing real-life patient care scenarios through advanced technology, while providing us with the ability to offer immediate feedback on how to best manage patient care scenarios that are faced every day.”
Ohio State College of Medicine is developing VR technology to further educate medical students and professionals on how to assess mass-casualty situations, such as shootings or bombings: The program, which is the result of a five-year, roughly $1.8-million grant from the Agency for Healthcare Research and Quality, is expected to roll out within the next one to two years, Douglas Danforth, academic program director at the Ohio State College of Medicine, said. The new VR simulation — led by Danforth and his co-principal investigator Nicholas Kman, an emergency medicine physician at the medical center — will show trainees ranging from medical students to EMTs a subway bombing scene with multiple victims. The user is responsible for acting as a first responder who determines the extent of the patients’ injuries, as well as takes the appropriate steps to treat them if necessary. The simulation also gives the “first responder” access to a medical bag with several tools such as tourniquets and triage tags, Danforth said. Danforth said simulation users will practice triage, the process of assessing a large number of injured people and determining in what order to treat them. “Each trainee is expected to triage and treat every patient in the scene using the Sort-Assess-Lifesaving Interventions-Treatment or Transport (SALT) triage system,” Kman said in an email. “While implementing SALT Triage, trainees must also identify which lifesaving procedures are appropriate for each patient.”
Sponsored Content:
UIC Opens New Simulation And Integrative Learning Institute For Medical Students: Director of Simulation Dr. Christine Park showed WBBM Newsradio one of the mechanical patients at the Simulation and Integrative Learning Institute. There are also human actors who will take on various roles to help the students learn. The Simulation and Integrative Learning Institute has exam rooms, inpatient rooms, and an operating room among its 28,000-square feet of space. Dr. Park said it’ll help medical students to keep up with the latest advances. “Healthcare is quickly changing, so yeah, you have to learn new skills as they come onto the market,” she said. Dr. Park compares the simulation training to what’s regularly required in commercial aviation. “If you don’t simulate, you don’t fly. These are for trained, practicing pilots,” she said.
Unveiling shows VA’s simulation work to provide better Veteran care: This interaction displayed the latest simulation center for improving Veteran care, unveiled in September at the Hunter Holmes McGuire VA Medical Center in Richmond, Virginia. “We want to make sure everyone is trained to a standard,” Wiltz said. “That’s the key to zero harm, high reliability healthcare, earning the trust of Veterans.” As an example, Wiltz said a cardiac arrest victim is 50% more likely to survive at a VA medical center. He said a study showed the increased survival rate was due to standardized training, which is one of the main goals of simulation. VA currently has a network of 12 advanced certified sites. Wiltz said these sites are doing the “biggest and best of simulation” for VA, including virtual reality training and video training. Instead of sitting behind a screen completing computer-based training, healthcare providers can learn skills through hands-on and live-action demonstrations.
Osso VR Partners with Sawbones: Osso VR, a validated virtual reality (VR) surgical training platform, is partnering with Sawbones, the originator of “hands-on” orthopedic and medical workshop models worldwide. Together, they’re digitizing Sawbones’ traditional bone models to expand and diversify the products’ application, enabling the models to be used repeatedly and without barriers in the virtual environment.
Students at A.R. Johnson use virtual reality for CPR training: “You’ve heard something crash outside,” Dr. Palladino shares some of the scenario students read before the CPR lesson. . “You see a gentleman coming down the street who appears confused.” Student Jasmine Yancey describes how Thursday’s CPR lesson is part of a bigger project. “Our case is located in Haiti where an earthquake happened and we are treating the patients so we are acting as emergency medical responders because that’s what we’re going to be certified to be towards the end of the class,” Yancey says. “They had to triage the patients,” Dr. Palladino shares more about the course. “They’ve had to figure out agencies that they could contact to get resources, but now we’re going to move into some training on individual patient care.”
Subscribe to Our Newsletter for More Great Simulation Updates!
Lance Baily, BA, EMT-B, is the Founder / CEO of HealthySimulation.com, which he started in 2010 while serving as the Director of the Nevada System of Higher Education’s Clinical Simulation Center of Las Vegas. Lance also founded SimGHOSTS.org, the world’s only non-profit organization dedicated to supporting professionals operating healthcare simulation technologies. His co-edited Book: “Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice” is cited as a key source for professional certification in the industry. Lance’s background also includes serving as a Simulation Technology Specialist for the LA Community College District, EMS fire fighting, Hollywood movie production, rescue diving, and global travel. He and his wife live with their two brilliant daughters and one crazy dachshund in Las Vegas, Nevada.
Sponsored Content: