Northwestern University Simulation-Based Mastery Learning Course
Researchers at NorthWestern Simulation, a leading medical simulation program under University Feinberg School of Medicine, have developed a simulation-based mastery learning (SBML) approach to assist simulationists/educators in training healthcare providers through competency-based education. Training using SBML has demonstrated improvements in patient care outcomes in multiple studies. This HealthySimulation.com article by Jeffrey H. Barsuk, MD, MS, Marsha Hawk, RN, MS, EdD, and Diane B. Wayne, MD will discuss SBML to train medical professionals and improve patient care, and share about an immersive “how to” SBML course available at Northwestern University Feinberg School of Medicine.
Research shows that when rigorously assessed, nurses, physicians, and advanced practice providers (APPs) exhibit wide variability in clinical skills. This variability, often in the face of vast clinical experience, can result in patient harm. Gaps in clinical skills have been demonstrated in areas such as patient communication, teamwork during cardiac arrests, laparoscopic surgery, anesthesiology emergencies, central venous catheter insertion and maintenance, IV insertion, operative vaginal delivery, and many more. The way health professions faculty traditionally educate and evaluate learners in the health professions is a key contributor to these variabilities.
Competency-based education is widespread but needs to be optimized to ensure that clinicians and patients benefit. Nursing and medical schools incorporate Entrustable Professional Activities (EPAs) into evaluating student preparedness, and graduate medical education uses Milestones to track resident and fellow performance. Using these tools optimally and fairly requires faculty development, interrater reliability, and rigor. Too often, the clinical skills of health professions students and trainees are assessed using chance experiences and their supervisors’ subjective impressions. This leads to summative evaluations that may be biased or based on unreliable data.
Sponsored Content:
https://www.youtube.com/watch?v=oFuIRK-17ss&vq=hd1080
In one study, a Northwestern University Feinberg School of Medicine research group evaluated graduating neurology residents. The researchers compared the residents’ final graduating Milestone performance score for treating status epilepticus (a neurological emergency) to a rigorous evaluation of their skills in a simulated setting. Residents’ graduating Milestone performance scores rated by their faculty were all in the “competent” range in managing this emergency and ready for independent practice. Yet, when assessed during a simulated status epilepticus scenario, graduating residents performed poorly, and their Milestone ratings did not correlate with actual performance.
Hospital credentialing is another area ripe for improvement. Most hospitals allow physicians and APPs to perform a procedure based on a set number of prior procedures performed on patients. However, multiple studies have shown that clinical experience is not a proxy for skill.
A Northwestern University Feinberg School of Medicine research team evaluated the simulated central venous catheter (CVC) insertion performance of experienced attending physicians (critical care, emergency medicine, anesthesiology, and internal medicine) with current hospital privileges to perform the procedure. Despite the vast clinical experience, only 12 of 67 (17.9%) completed an internal jugular CVC insertion proficiently, and only 11 of 47 (23.4%) performed a subclavian CVC insertion proficiently.
Sponsored Content:
How Can Simulation-based Mastery Learning Improve Clinical Skills?
Health professions education schools, residency and fellowship programs, and hospital systems can change their approach and use reliable data to make valid decisions about their students’ and clinicians’ ability to perform procedures and skills. Using SBML is a tested and proven solution. SBML is an extreme form of competency-based learning where all participants are required to meet or exceed a minimum passing standard (MPS) on a simulator before completion of training. The MPS is set at a level that provides independent, safe, and effective patient care. Participants who do not meet the MPS undergo further deliberate practice until they can be retested and subsequently meet or exceed this score.
Typical SBML curricula start with a skills or knowledge pretest to establish a baseline. If participants reach the MPS on the pretest (rare), they do not need to complete the rest of the curriculum. However, if they do not meet the MPS, participants observe standardized lectures and “how to” videos. Next, they undergo deliberate practice on the simulator with an expert instructor. Finally, they take a posttest where they are all required to meet or exceed the MPS. In SBML, learning time varies, but educational outcomes are uniform. SBML improves clinical skills in communication, teamwork, and various procedural skills. SBML also improves patient care outcomes in IV insertion, CVC insertion, paracentesis, thoracentesis, laparoscopic common bile duct exploration, and after Advanced Cardiac Life Support events.
SBML was developed at Northwestern University Feinberg School of Medicine in 2003. Northwestern faculty use SBML widely to help assess and document procedural skills, teamwork, and communication. Our hospital also uses SBML when granting certain privileges to internal medicine physicians. Our cumulative and sustained research program with over 100 peer-reviewed publications and a 2020 textbook has shown that SBML is a vital tool to help rigorously assess students, residents, attendings, and nurses and improve patient care outcomes. Protocols developed at Northwestern are currently used worldwide to improve education and patient care.
Immersive Simulation-Based Mastery Learning Course Available Now
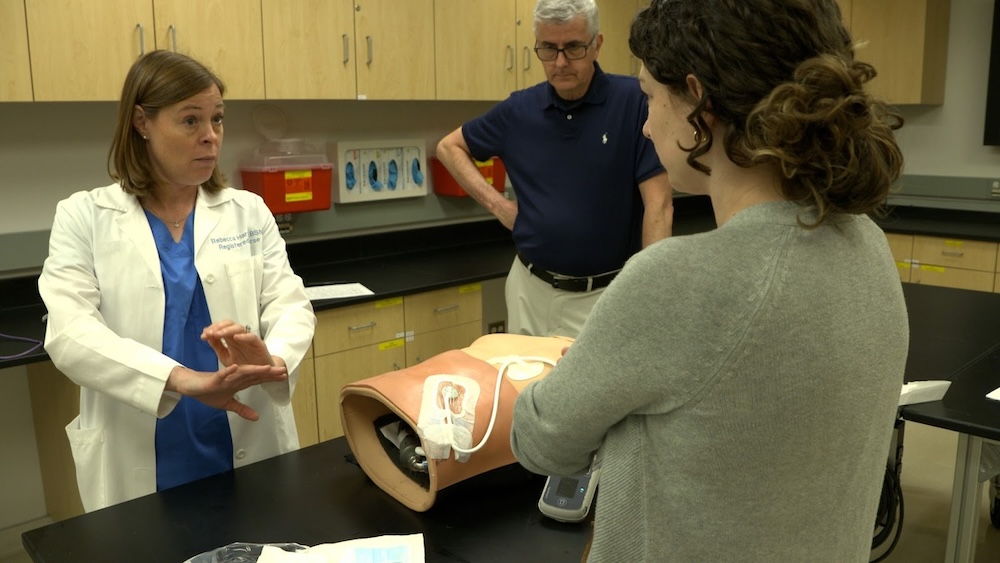
To share the learned experiences, Northwestern Simulation developed an immersive continuing education SBML course. The course focuses on creating and implementing SBML curricula. After participating, attendees worldwide have developed, instituted, and published outcomes on SBML interventions. Join Northwestern University Feinberg School of Medicine’s Simulation Center Faculty in Chicago to learn more about this approach.
Participants are encouraged to bring a current existing curricular idea or create a novel SBML curriculum in their school or hospital. Key faculty experts include the creators of SBML – Drs. William McGaghie and Jeffrey Barsuk (course co-directors), and Dr. Diane Wayne. Other course instructors have extensive experience with SBML and include Drs. Mark Adler, Celia O’Brien, Eric Hungness, David Salzman, Julia Vermylen, and Gordon Wood. The next three-day immersive SBML course will be held on March 4-6, 2024.
More About Northwestern Simulation
Northwestern Simulation is located on a 30,000-square-foot state-of-the-art facility on the Northwestern University Chicago campus. The simulation space trains learners in diverse areas of care delivery ranging from outpatient clinic visits to inpatient encounters in med/surg, intensive care, emergency room, OB/Gyne, and surgery. The space also contains an innovations laboratory where a full-time engineer builds and repairs simulators. A virtual reality room has computerized simulators that immerse learners in a simulated procedural skills training environment. Northwestern Simulation has an audiovisual system wired throughout the center, allowing for session recording, capture, and live and archived remote viewing.
Learn More About Northwestern’s Simulation-Based Mastery Learning Courses!
Jeffrey H. Barsuk, MD, MS, SFHM is the Robert Hirschtick Professor of Medicine and Medical Education at Northwestern University Feinberg School of Medicine. He graduated Alpha Omega Alpha from Northwestern University Feinberg School of Medicine and completed a residency in Internal Medicine at the McGaw Medical Center of Northwestern University at Northwestern Memorial Hospital. He completed a Master’s of Science Degree in Clinical Investigation. He also completed a certificate program in Healthcare Quality and Patient Safety. Dr. Barsuk serves as the Executive Medical Director of Northwestern Simulation for Northwestern University Feinberg School of Medicine. Dr. Barsuk focused the last 19 years of his research on optimizing physician, advanced practice provider, nurse, and patient clinical performance using simulation technology. These efforts have been based on the mastery learning theoretical framework, and his research team uses rigorous, validated standards for healthcare provider training. His team has published over 100 articles on this topic that demonstrate how this training approach improves clinical skills and patient care and outcomes while lowering healthcare costs. Additionally, his research group has recently published a book entitled, Comprehensive Healthcare Simulation: Mastery Learning in Health Professions Education. Dr. Barsuk’s research has been funded by several private and government organizations including the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Barsuk is recognized internationally as a researcher in medical education and patient safety. He has been given awards from the Society of Hospital Medicine, Association of American Medical Colleges, and the Society for Simulation in Healthcare. He is sought internationally to lecture on how the use of simulation-based medical education improves patient safety.
Sponsored Content: