Implementing Curriculum Using Simulation To Augment Pediatric Emergency Medicine Rotation
This Med Ed Online article “Development and assessment of a pediatric emergency medicine simulation and skills rotation: meeting the demands of a large pediatric clerkship” by Elaine K. Fielder and colleagues can help us expand simulation into our programs.
Objective: To implement a curriculum using simulation and skills training to augment a Pediatric Emergency Medicine (PEM) rotation within a pediatric clerkship.
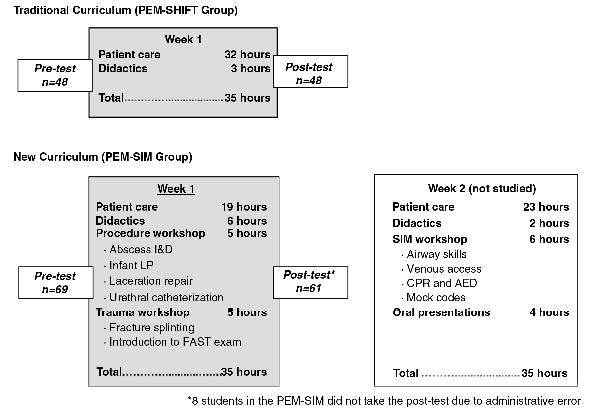
Background: PEM faculty are often challenged with a high learner to teacher ratio in a chaotic clinical setting. This challenge was heightened when our pediatric clerkship’s traditional 1-week PEM rotation (consisting of 4 students completing four 8-hour ED shifts/week) expanded to 8 students every 2 weeks. We sought to meet this challenge by integrating simulation-based education into the rotation.
Sponsored Content:
Methods: Clerkship students from March to June 2012 completed our traditional rotation. Students between July and October 2012 completed the new PEM-SIM curriculum with 19 hours ED shifts/week and 16 hours/week of simulation/skills training. Pre/post-tests evaluated 1) medical management/procedural comfort (five-point Likert scale); and 2) PEM knowledge (15 multiple-choice questions).
Results: One hundred and nine students completed the study (48 traditional, 61 PEM-SIM). Improvement in comfort was significantly higher for the PEM-SIM group than the traditional group for 6 of 8 (75%) medical management items (p<0.05) and 3 of 7 (43%) procedures, including fracture splinting, lumbar puncture, and abscess incision/drainage (p<0.05). PEM-SIM students had significantly more improvement in mean knowledge compared to the traditional group (p<0.001).
Conclusions: We have successfully integrated 16 hours/week of faculty-facilitated simulation-based education into a PEM rotation within our clerkship. This curriculum is beneficial in clinical settings with high learner to teacher ratios and when patient care experiences alone are insufficient for all students to meet rotation objectives.
Read the full article on Med Ed Online!
Sponsored Content:
Lance Baily, BA, EMT-B, is the Founder & CEO of HealthySimulation.com, which he started while serving as the Director of the Nevada System of Higher Education’s Clinical Simulation Center of Las Vegas back in 2010. Lance is also the Founder and acting Advisor to the Board of SimGHOSTS.org, the world’s only non-profit organization dedicated to supporting professionals operating healthcare simulation technologies. His co-edited Book: “Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice” is cited as a key source for professional certification in the industry. Lance’s background also includes serving as a Simulation Technology Specialist for the LA Community College District, EMS fire fighting, Hollywood movie production, rescue diving, and global travel. He and his wife Abigail Baily, PhD live in Las Vegas, Nevada with their two amazing daughters.
Sponsored Content: