How to Champion Integrating Clinical Simulation into a Curriculum
Medical simulation is one of the highest-impact components of modern clinical education. Despite this reality, integrating this training methodology as a regular part of a curriculum often presents a challenge, especially when some in academia still struggle to see healthcare simulation’s importance. This article serves as a field guide to promoting this integration with tactics like becoming familiar with research, aligning to didactic content, developing Mini-Champions and getting smart about showing data. For highest impact, these efforts should be directed towards the faculty who are designing the curriculum and other decision-making institutional stakeholders.
Simulationists are used to seeing learners experience critical “Aha!” moments, which leave little doubt in their minds about just how effective clinical simulation is. As such, one of the biggest temptations is to be louder about these stories than actual research, which is the ruling language of academia. The priority must be to communicate the evidence first, but the point may be driven home by highlighting the simulationist’s real-world observations.
While the world of evidence can seem intimidating, this does not mean needing to know all the existing research right off the bat. An easy place to start is by finding the research directly relevant to the specific blockers that prevent more institutional usage of clinical simulation.
Sponsored Content:
If the issue is a lack of belief that healthcare simulation adequately complements clinical rotations, reference the NCSBN’s landmark study on the replacement of clinical hours with nursing simulation. (1) Alternatively, other studies show how simulation-based education (SBE) affects real world outcomes (2) or clinical simulation’s impact on performance in OSCE’s. (3) After becoming more comfortable with interpreting and applying research findings, the next step might be to execute smaller, local studies to show how findings apply to your specific learners.
Applying a Curriculum Needs Assessment for Healthcare Simulation
Sometimes clinical simulationists gravitate towards deploying scenarios that they enjoy or are knowledgeable about. However, this approach of building out a suite of clinical experiences has potential to overlook important aspects of the curriculum. As such, the medical simulationist should always start with a Needs Assessment in which they identify which learning outcomes are most relevant to the curriculum.
A great way to begin doing this is by meeting with faculty, combing over the syllabus, identifying where learners tend to struggle and consulting on how a well-timed and thoughtfully approached scenario could be used to meet the desired competencies. Offer a trial run and reconnect afterwards to identify whether the goals truly were met.
Sponsored Content:
Getting Laser-Focused Data out of Healthcare Simulation
Following on from the above point, one cannot measure what they do not first define. Implementing a trial run for a clinical simulation won’t mean much if everyone doesn’t agree beforehand about how the medical simulation’s impact will be measured. Once the specific learning outcomes have been defined, a point can be made to collect that data throughout the clinical simulation’s delivery.
Examples of how this could look in practice could involve implementing a disease-specific competency checklist, pre- and post-simulation quizzes or aligning the learners’ performance in clinical simulation to their performance in clinical rotations. If any of these elements will include using observers to document learners’ attainment of competencies during the sessions, be mindful of the availability of relevant faculty or clinical instructors.
The Importance of Voluntary Utilization and Mini-Champions in Healthcare Simulation
Learners often request more opportunities to practice clinical simulation. While the reasons for this are typically obvious to the simulationist, they may not be for stakeholders and decision-makers. Capturing these requests and any subsequent additional clinical simulation delivered can go a long way in proving demand for those directly influencing the curriculum.
Beyond merely tracking the number of times this occurs, the simulationist should be sure to capture “the why” behind those learners’ requests, focusing on qualitative feedback like improved confidence, competence and practical examples of how clinical simulation has helped them excel. This approach can not only help to measure and report these elements, but to encourage learners in articulating how medical simulation works to improve outcomes – and ultimately transform them into Mini-Simulation Champions!
Best Practices in Communicating Findings in Healthcare Simulation
All of the tactics above represent significant clinical simulation “ammunition,” but communicating these findings effectively is more critical than the findings themselves. See below for a few quick tips on getting high-impact results from the data that’s been gathered on research, curricular needs, pilot data, utilization and learner feedback.
- Be ready with cliff notes: Detailed reports are completely appropriate considering all of the information that’s been collected, but academics are busy and may not dive into the full analysis. Have the highest-impact findings memorized and ready to show off at any encounter with stakeholders.
- Get visual: Data visualization can be far more powerful than written text in communicating results.
- Tell, tell and tell again: Communicating these findings just once won’t be enough, especially in the information-rich context of academia. Search for every opportunity to show how clinical simulation could have a larger impact on curriculum, from poster presentations to regular faculty meetings to invitational luncheons and everything in between. Never forget that the squeaky wheel gets the oil.
Learn More About Clinical Simulation
References:
- Hayden, J. K., Smiley, R. A., Alexander, M., Kardong-Edgren, S., & Jeffries, P. R. (2014). Supplement: The NCSBN National Simulation Study: A Longitudinal, Randomized, Controlled Study Replacing Clinical Hours with Simulation in Prelicensure Nursing Education. Journal of Nursing Regulation,5 (2), C1-S64.
- Meyer, Mary N. RN, MSN; Connors, Helen RN, PhD; Hou, Qingjiang MS; Gajewski, Byron PhD The Effect of Simulation on Clinical Performance, Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare: October 2011 – Volume 6 – Issue 5 – p 269-277 doi: 10.1097/SIH.0b013e318223a048
- Nuzzo A, Tran-Dinh A, Courbebaisse M, Peyre H, Plaisance P, Matet A, et al. (2020) Improved clinical communication OSCE scores after simulation-based training: Results of a comparative study. PLoS ONE 15(9): e0238542. https://doi.org/10.1371/journal.pone.0238542
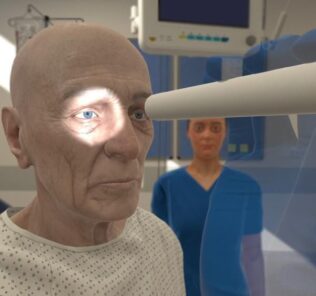
Nathan Costiuc, MSN, APRN, FNP-BC, is a Nurse Practitioner and Healthcare Simulation Educator. He began his career delivering clinical simulation to nursing students, quickly realizing the industry’s potential to impact modern training for all healthcare professionals. In navigating better ways to deliver clinical simulation, Costiuc entered into the world of virtual reality, and now works as a Clinical Education Specialist for Oxford Medical Simulation. His passion is in using innovative methods and emerging technologies to reduce medical error, solve practical problems, and improve patient care. He also actively works with disabled veterans in the clinical setting.
Sponsored Content: