Simterviews: Medical Simulation Experts Discuss COVID-19 Responses
The coronavirus pandemic created a number of challenges for the field of simulation since the virus’s onset in March 2020. Simulation centers, institutions and vendors across the world were forced to reevaluate their protocols and procedures, and many were forced to temporarily close their doors until such standards were finalized and approved.
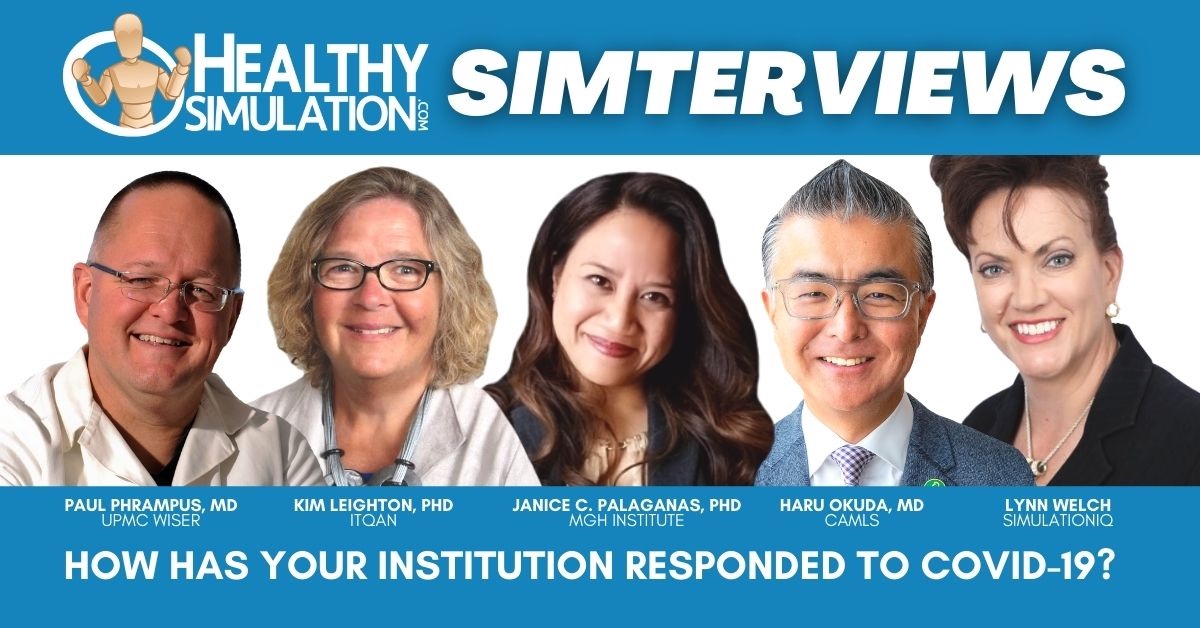
HealthySimulation.com spoke to a number of healthcare simulation experts about the pandemic during the website’s new Simterviews series. Throughout this series, many of these experts described how their institutions have responded to COVID-19, and what obstacles and opportunities were presented as a result.
Sponsored Content:
Dr. Paul Phrampus, MD, Director of the Peter M. Winter Institute for Simulation, Education and Research (WISER), and professor in the Departments of Emergency Medicine and Anesthesiology at the University Of Pittsburgh School Of Medicine.
Dr. Paul Phrampus: WISER is in a situation where we responded to COVID-19 in a number of ways. We are committed as an institution to believe that simulation is absolutely essential. We at the University of Pittsburgh and the UPMC Health System have wrapped simulation in the quality, care and safety of all of our patients at our 30-plus hospitals. That’s a challenge because we can’t just say “OK, turn it off, pause.”
We have taken advantage of the description caused by COVID-19 to reevaluate what we are doing, how we are doing it and how we can continue training but reengineering some of our old ideas to realign with basic concepts of COVID-19 safety: social distancing, masking, spreading out classrooms and changing the studio-to-instructor ratio in classes. We’ve also held a number of seminars for the SSH, talking about our efforts to pioneer remote healthcare simulation. We’ve been working on remote simulation for a long, long time. We’ve had a few posters at IMSH over the years.
I think COVID-19 really sped that up and pushed us to use off-the-shelf technology like Zoom to a different level to be able to accomplish simulation training. We’ve been doing some clinical simulation all the way through the pandemic experience. The other thing WISER was positioned to do, because we are a research and investigation facility as well, is analyze using simulation to spin up some devices that actually went to market and became products as different safety solutions for both providers and patients as they are cared for during the pandemic.
Sponsored Content:
Kim Leighton, PhD, RN, CHSOS, CHSE, ANEF, FAAN. Executive Director, ITQAN Clinical Simulation & Innovation Center in Doja, Qatar. She is the founder of the Evaluating Healthcare Simulation website, and is respected as a simulation educator, researcher, and mentor.
Dr. Kim Leighton: We’re hospital-based and initially the Sim Center was completely closed. I held off about two weeks, then I petitioned Infection Control to let me reopen. Then we started to do COVID-related training and that’s all we did. My organization is a government facility that covers all of the country. During COVID we opened 37,000 isolation beds, 12,500 quarantine beds, 3,000 acute care beds and another 750 ICU beds. That’s about 50,000 more beds than we initially had.
However, the airport is still closed, so it became a question as to where we were going to get the nurses and the other staff to take care of all these patients. We also have one of the highest per capita infection rates in the world across our population of about 2.7 million. We’re getting close to 130,000 cases with a high percentage of positivity. Our numbers are now going down, but immigration remains closed.
The way we managed the surge was to “upskill,” and we trained 450 outpatient nurses in our Sim Center and a couple of quarantine hospitals to be ICU nurses to take care of COVID patients. We sent manikins to the quarantine hospitals so that they could train on-site. Now, because those 450 outpatient nurses are still working in the hospital, we need to reopen outpatient services. In order to do that they are now going to train office staff to be patient-care assistants to work in the outpatient facilities.
Our Sim Center has provided the support for all those trainings. The ER doctors and anesthesia had to learn some new airway management techniques. We have been running every day since we reopened. During the high surges of COVID infections we staged it though, and anyone on my team who could work from home and I staffed according to building activities.
Now we’re all back to work and we can feel that it is getting busier and busier because all the non-COVID things that were cancelled, people want to do that again. The challenge is maintaining a safe work environment for everyone and ensuring that COVID policies and procedures are adhered to so we can stay healthy.
Janice C. Palaganas, PhD, RN, NP, ANEF, FNAP, FAAN, FSSH is the Associate Director of Health Professions Education at MGH Institute of Health Professions and Principal Faculty at the Center for Medical Simulation (CMS). She develops health professions educators in an Integrated Programming Environment setting.
Dr. Janice C. Palaganas: Like everyone else, we have gone online. We’ve always been an online program, so that is not new to us. I think there was good and bad to our online status. The good thing is we were already doing it. We know what it’s like. The bad thing is everybody started calling us and asking for our help and asking us to teach them. You want to help everyone, so there was a little bit of slowdown just by helping other people. We did a lot more podcasts to get out some more information and try to share some tips and techniques.
Our MGH IHP has been just amazing in terms of the COVID-19 response as an organization. By that I mean caring for their employees and caring for the students and creatively thinking of approaches for clinical placements and online learning to address needs as they arise. It was very hard to get one step ahead, but our leadership worked tirelessly to make sure that they were caring for everyone. This was really wonderful in terms of simulation.
I live online. I’m a techie at heart and it was so difficult trying to get some things online initially, like programs. It was also hard to get online education launched, and to get leadership buy-in. I think the pandemic made that push for those of us that we’re really trying to create online programs. I think the most fantastic thing that I saw during the coronavirus pandemic was watching educators who were hesitant and scared and didn’t have a preference for online learning find a love for it. That’s been very interesting and exciting. In some ways COVID-19 really pushed us and sped up a process that would have taken 10 years to get to.
Dr. Haru Okuda, MD, FACEP, FSSH, is the executive director of University of South Florida Health’s Center for Advanced Medical Learning and Simulation (CAMLS). In this role, he has oversight of a 90,000-foot, state of the art, advanced training facility, with the mission of creating and providing experiential learning that improves clinical skills and patient care in the community and around the globe.
Dr. Okuda: At Tampa General Hospital, there was a need and we responded. Our team stepped up to develop and run training for front line healthcare teams at our level and trauma center that are affiliated with CAMLS.
If you’ve never been to CAMLS, we’re a 90,000-square-foot, three-story, free-standing simulation center in downtown Tampa. In 2012 when it opened, it was probably the largest simulation center in the country. I know there are many others that are much bigger now, but our focus is on two groups of trainees. One is the students that are at USF Health. This includes pharmacy medicine, nursing and public health professionals. We also have external clients, including scientific organizations and the American College of Emergency Physicians. In March, we shut down CAMLS, just as everybody else shut down their operations. During that time we created efficiencies and safety protocols that we needed to be able to reopen. As I mentioned, these are critical things that need to occur for training.
Even though we don’t deliver direct patient care, I feel passionate about what we do, and that if we don’t do it, people will suffer. Medical errors would increase and team training would get worse. We knew that we had to create an environment which was safe for our learners, our staff and our facility. We had to be up and running and ready to go when it was time to go. We worked really hard with our team through March, April and May while we were running the Tampa General Hospital training to be prepared for launch in June. We have hundreds of residents that come through CAMLS every year that need to go through our boot camps. They needed this training before they started taking care of patients for the first time as residents. We opened our doors in June and we were extremely successful.
We had no COVID-19 cases during July. We’ve been very solid in our safety protocols with COVID-19, and we were able to train hundreds of residents. Eventually the medical students returned, and now our external clients are coming back because of our safety protocols. We’re very fortunate in that we have such a large simulation center, that even if we’re at a capacity of 30% or so for training, we could still have hundreds of people come through because it’s such a big center. We’ve been very agile, flexible and innovative in how our team has brought the training together. We’ve been able to move forward since COVID-19.
Lynn Welch is the vice president of business development and marketing at Education Management Solutions, now SimulationIQ. She has also served as a Board of Director At Large Member and corporate roundtable chair at the Society for Simulation in Healthcare (SSH) since January 2020. Her unique background includes federal defense, global marketing, business development, sales leadership, and volunteer efforts.
Lynn Welch: We have done a lot of innovation around again serving the need for healthcare simulation training without brick and mortar centers, focusing on (the question of) how do you deliver clinical simulation by proxy? We came out with a product called Distance SIM, which allows an instructor to go into a brick and mortar sim room even if their students can’t be there. The student can remotely be right in that room with the instructor, seeing through the cameras, seeing everything happening in the room and directing a proxy to take actions on a hands-on physical exam using a mannequin or other tools, removing that wall. That was one of the pieces we worked on.
We also looked at the patient exam, and we built a full turnkey, virtualized (objective structured clinical examination) format. We had an online platform that would facilitate all the requirements for a high intensity OSCE exam and allow for that fully virtual telemedicine-enabled exam, virtual exam. Live, standardized patient instructors and observers can log in, watch live and evaluate if it’s all scored — just like it would be in their healthcare simulation center, but a hundred percent virtual.
We deployed that inside of two weeks. We had a client this summer who engaged with our virtual OSCE platform, right before the Fourth of July. Our development team stood it up for them over the July Fourth weekend. We trained all of their instructors over the next three days, and in the beginning of August they ran a giant day of clinical simulation where they conducted 1243 OSCE encounters across their four medical school locations. They were all training together, keeping everything moving forward, and were able to have it happen inside of two weeks. If you think about the timelines for an initiative like this in the past, you’re talking months, and this is now happening in the matter of weeks. When you can accelerate these timelines and get these products fully developed, fielded and deployed, then there’s no limit on what we can do in the future.
Subscribe Now for More Great Simterviews!

Simterviews: Dr. Kim Leighton | Executive Director, ITQAN Clinical Simulation & Innovation Center

Simterviews: Medical Simulation Expert Interviews | UPMC Director for Patient Safety, Dr. Paul Phrampus – Part 2

*NEW* Simterviews: Healthcare Simulation Interviews | UPMC WISER Center Director, Dr. Paul Phrampus – Part 1
Lindsey Nolen is the Content Director for HealthySimulation.com. She is an award-winning journalist with years of experience writing about the many different facets of healthcare, including clinical simulation education and training. She also helped create content for the healthcare career information website, CareersinHealthcare.com.
Sponsored Content: