Designing Prehospital Medical Simulation Scenarios
Written by David Halliwell –MSc. Paramedic, FIfL, Lizzie Ryan, MEd, MBA, MSc, RN, FIfL & Paul Jones, BSc (Hons) Cert Ed Paramedic. Shared with Permission.
Pre Hospital use of scenarios in paramedic education
Sponsored Content:
Key Words: Pre-hospital, Education, Simulation, Technical Competence, Practical Competence, Logistical Competence, Scenario Competence.
Background
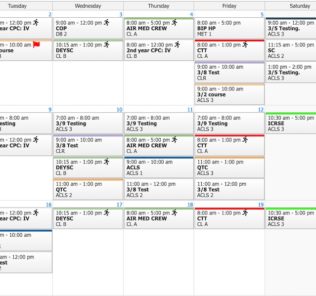
The team in Southwestern Ambulance NHS Foundation Trust (SWAST) has been evaluating various methods to decrease the numbers of failures within student paramedic practical examinations, and have for some years developed strategies for enhanced student experience and performance. This paper reviews a new paradigm for paramedic scenario-based education focusing upon the increased role of the tutor knowledge, and the enhancement of the importance of understanding logistical concerns in pre hospital care.
The Theory: Setting the scene
Sponsored Content:
This paper outlines the methods used to develop a model for the use of training simulation in pre hospital care using case studies undertaken within a United Kingdom (UK) ambulance service and suggests a new paradigm for teaching emergency care to ensure increased performance.
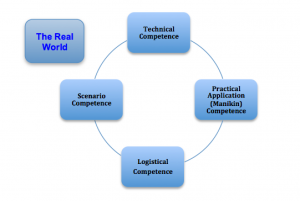
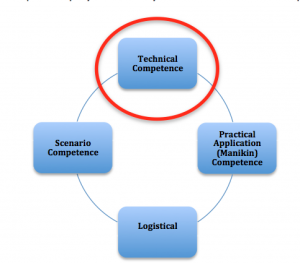
Fig 1: The Basic Concept (Halliwell et al. 2012)
The paper outline the four stages that should be considered by tutors before their students are exposed to clinical scenarios for educational purposes. These stages of paramedic education are relatively unique since the teaching and understanding oflogistical considerations are not necessarily a significant concern to other clinicians from wider health disciplines. In pre-hospital care our role includes the movement of patients and creation of access to patients, who may be trapped or requiring us to work within a confined space, in order that we can deliver our care (fig. 1).
More About the Authors:
David Halliwell –MSc. Paramedic, FIfL. David was the Head of Education for Southwestern Ambulance NHS for the last 8 years, having previously been a senior resuscitation officer, and paramedic for the last 20+ years. David has recently moved to the Middle East as Managing Director for Prometheus Medical (MENA), assisting with Paramedic and skills development throughout the Middle East and is currently completing his PhD in paramedic education.
Lizzie Ryan, MEd, MBA, MSc, RN, FIfL is the Education Business Manager of South Western Ambulance Service NHS Foundation Trust, and is a registered nurse. She is an educationalist and her role involves the development of higher education links for paramedic development and clinical leadership and management in her Trust. She is also a lecturer practitioner for the Open University, Bournemouth, Plymouth and Loughborough Universities, and is currently completing an EdD.
Paul Jones, BSc (Hons) Cert Ed Paramedic has been the Programme Lead for South Western Ambulance NHS Trust for the past 5 years. Though no longer the Bournemouth University Programme Coordinator for their FdSc Paramedic Science Programme, he remains as a lecturer practitioner and lead for the BSc (Hons) Emergency and Urgent Care Programme. Paul has been in the ambulance service for the past 20+ years and continues to develop vocational and higher educational courses for paramedics.
The First Stage of the Paradigm: Technical Competence (fig. 1)
Before attempting to run any clinical scenario or simulation the tutor must ensure that the student has the technical competence and clinical knowledge to perform the skill or task, otherwise the scenario will be setting the student up to fail, and may be seen as a pointless exercise and we would not be achieving our objective. This is referred to by the Authors as the ‘How’, ‘Why’ and ‘Who said’ of healthcare.
Understanding the ‘how’ and ‘why’ of healthcare is vitally important, and the authors believe that the Tutors role in ensuring accuracy of information, and having the ability to transmit the information in a method that is clearly understood by the student when teaching any information is key (fig. 10).
The ‘who said’ of healthcare is the understanding of the underlying evidence, and the technical evidence, that underpins our profession. This is sometimes lacking in pre-hospital care, certainly in the UK, and it is only in recent years that UK Paramedics and Ambulance practitioners have been undertaking clinical research. Advances are being made, however, and existing paramedic resources are now being updated to include evidence bases, such as the revision of Nancy Caroline (2012).
Far too often, as senior managers with responsibility for deciding the future of failing students, we track the students performance and educational failures backwards from the point of failure to try and understand what may have gone wrong and establish why a student may have failed to perform. Occasionally we find ourselves in a position where our tutors don’t teach or know everything in the detail that they should have, and a failure in an assessment is linked to poor tutor knowledge rather than that of the student.
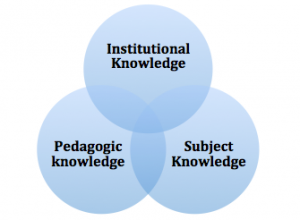
We don’t believe that we are unique in this finding as the quality of the education can be a determinant in the student’s future (Plato 1985). Banks et al (2000) described a simple construct model that tutors could use to develop their practice (fig. 2). This model indicates that teachers should ‘know their stuff’ (subject knowledge), ‘know how to teach their stuff’ (pedagogic knowledge) and know how to teach stuff’ in their institution (institutional knowledge) (p.23). The rapidly changing technological base that they are working from affects the design of the teaching process and the tutor knowledge.
Fig 2: A simple construct model for tutors to develop their practice in teaching students (adapted from Banks et al. 2000)
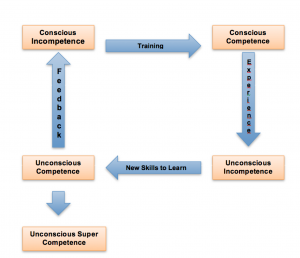
This concept can be linked to those found in research relating to the unconsciously incompetent proposed by Howell (1979, 1982), who described four elements of gaining competence. The first element is that of unconscious incompetence where the student’s perception is that they are not making any errors, but in reality they are making mistakes that they do not know about; here accurate feedback from the tutor is essential if practice is to be improved or changed. Unfortunately the Tutor may have some responsibility for this, and the errors may be due to the fact that the tutor themselves have not been taught correctly, and simply do not know any better, or have misinterpreted the information that was provided. If we have unconsciously incompetent tutors there is a chance that the wrong information or poor practice may be passed on to students, and a cycle of poor performance could be reinforced.
Next comes conscious incompetence where the student becomes aware of the errors and shortfalls in their knowledge, but is not sure how to address them; here accurate and effective training is key. The third element describes conscious competence where the student develops an understanding and begins to know what to do, and can differentiate between what works and what does not; here the students develops and hones their skills with experience and skills practice supported by the tutor. The fourth element describes unconscious competence with the student modifying their behavior and becoming intuitive (Ryan and Halliwell 2012). There is an advanced level described unconscious super competence when the performance is ‘effortless’ but this stage requires the input of reflective and evidence based practice, and a maturity of approach to the task (fig.3).
We suggest that often tutors teach the processes and procedures that they were taught, thereby reinforcing many of the myths in pre hospital care. This is not uncommon in education where the ‘see one, do one, teach one’ mentality may still exist.
Fig 3: The Human Learning Process Cycle (adapted from Palmer and Palmer 2007)
The Second Stage of the Paradigm: Practical Application (Manikin) Competence
The second stage in the process of reviewing the new paradigm for paramedic education is to review the creation of muscle memory through practice of skills, in this case, this concept is referred to as manikin competence; this name can be changed dependent on the task or activity being learnt. This occurs once the student has the technical ability and understanding; it is preferable to allow them the opportunity to practice their technical skills on manikins or skills trainers; first ensuring that they know how to use the simulation equipment (fig. 10). This stage is to create both physical dexterity, muscle memory (Krakauer and Shadmehr 2006), and assist with the building of mental bridges, and it can decrease the need for attention and create maximum efficiency in a skill; for example, practicing Cardio-pulmonary Resuscitation (CPR) in order to gain a feeling for the correct depth and rate of chest compression.
Muscle Memory
What does it mean to learn a new skill and go from ‘novice’ to ‘expert’ described by Benner (2001)? In the world of pre-hospital care this learning means memorising how to use our hands, and medical equipment in a coordinated way to save lives. But how does this memorising take place?
At first, we need to concentrate in order to make our hands, arms and feet move in just the right way, based on our perceptions of the event. What we’re learning is precision; i.e. how to make the correct depth of chest compression, or the appropriate technique of direct laryngoscopy without damaging the teeth.
Fine et al. (2002, Wolfe et al. 2009) have discovered that there are a large number of internal brain structures that work together with the input and output brain structures to form fleeting images in the mind. Using these images, we learn to interpret input signals, process them, and formulate output responses in a deliberate, conscious, way. But after a while, the ‘seeing-thinking-doing’ gradually becomes ‘seeing-doing’ because our muscles seem to ‘know’ and ‘remember’ just what to do. What we are learning now is speed, i.e. how to perform the task carefully and quickly. This is muscle memory (Krakauer and Shadmehr 2006), and Fine et al. (2002, Wolfe et al. 2009) often refer to this as ‘kinesthetic memory’ or ‘neuro-muscular facilitation’. This type of memory stays with us even if we do not practice it for a while; for example, riding a bike. Wolpert et al. (2011) also describe “sensory-motor” learning, since we are combining sensing input, i.e. what we see with our eyes, with motor output, i.e. what we do with our body, we gather the information and process the sensory information in order to carry out the action.
Of course, during the ‘drill-and-practice’ (Tomei 1998), our muscles aren’t really memorising anything, since all memories are stored in our brain; instead our brain interprets what we see and sends nerve signals to our muscles to make our body move. By making the same movements in response to the same visual cues over and over again, the associated nerve-muscle connections gradually become more effective, i.e. the transmission of the signals becomes more effective, and this is how the ‘thinking’ in the ‘seeing-thinking-doing’ process is gradually replaced by ‘seeing-doing’, i.e. by muscle memory. Della-Maggiore (2005) called this process ‘consolidation’, and describes it as the stabilising part of the process.
In the world of paramedicine muscle memory is especially important because it’s the combination of care and speed that make operators truly competent, or unconsciously competent (Howell 1979, 1982). In addition, muscle memory allows us to turn our attention to the ‘bigger picture’; for example, to plan the next step in the activity or event, by taking over a large part of our ‘cognitive load’ (Pass et al. 2004). This involves the load related to the control of the working memory, and during complex activities the ‘load’ of information and interactions can work to under or overload the working memory; so continuous practice of a skill is essential in building unconscious competence (Howell 1979, 1982).
But there’s a ‘catch’: to learn the new skills and acquire muscle memory, we must be practicing properly. This means effective feedback, right from the beginning of the learning process as novices do not know enough initially about doing things right to be able to notice, and correct, their own mistakes; the unconsciously incompetent (Howell 1979, 1982).
In addition, if they do not practice the skill or action properly, the student will continue to perform it incorrectly and they will then need to unlearn the skill or action practice in order to change any bad habits they have developed. Students need to have the ability to take a conscious control of their learning, and to be able to plan and develop their learning strategies and to monitor the effectiveness of them using self assessment and re-evaluation; then, and only then can they adjust their practice and reflect on the learning, this is called metacognitive awareness (Ridley et al. 1992). This helps them to be aware when they do something incorrectly and helps them to problem solve and apply reasoning to their actions (Scardamalia and Bereiter 1991). That’s why we strongly believe that ‘perfect practice makes perfect.’
Acquiring skills is variable. Some people learn faster than others and go on to achieve higher levels of performance just because they were born with more pre-requisite physical abilities. Some individuals acquire ability more easily than others; however, this could be due to a number of contributing factors, including motivational and personality influences as well as previous learning experiences. These contributory factors can equip a person with knowledge, attitudes, skills, and self-confidence (Perkins, 1981).
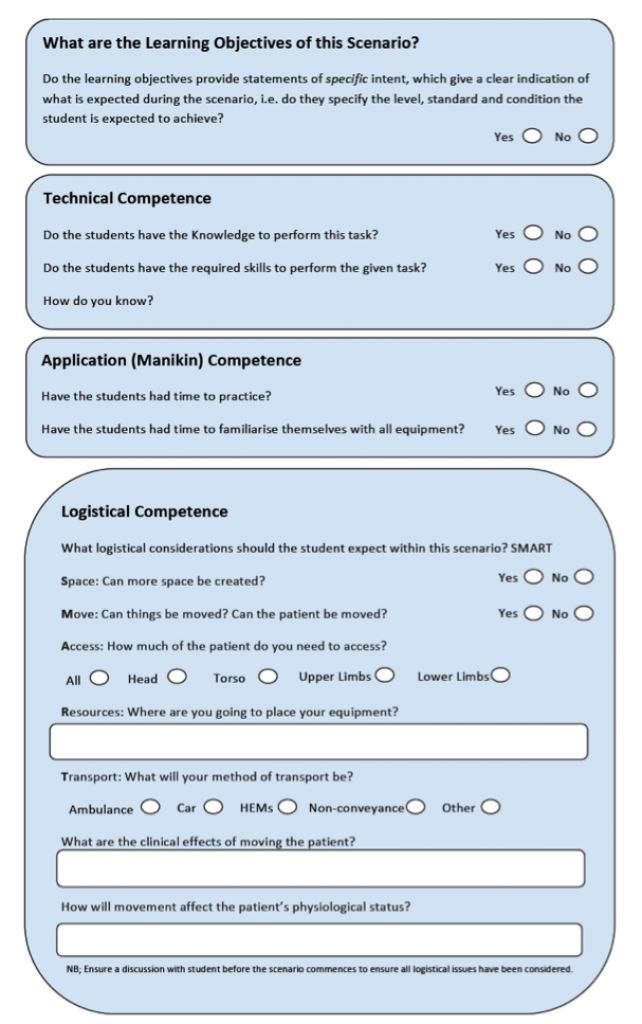
The Third Stage of the Paradigm: Logistical Competence
Pre hospital care is a unique part of medicine, since it involves many logistical considerations that students in other aspects of care do not need to worry about. Logistical considerations include: the need to create space; for example, the practitioner may need to move a patient out of the toilet where they have collapsed, creating access rather than trying to manage a cardiac arrest in a confined and dangerous space, or the methods used to move a peri-arrest patient from the bedroom of a house into the ambulance and on to hospital (fig. 10). What are the facets of moving the patient as regards the patient’s physiological status, and clinical effects of moving the patient post arrest? Should we sit a ROSC patient in a carry chair? Should they be brought down in a supine position? How is this best achieved (fig. 10)?
We encourage discussion of logistics prior to asking students to perform in complex clinical settings, since the student will be less likely to make mistakes if they have been given the opportunity to think through the practical and logistical problems that will affect their performance. The student should also be encouraged to consider the method of transport to be used including HEMS, Care, Ambulance, or non-conveyance (fig. 10).
Stage Four of the Paradigm: Scenario Competence
Once the student has the technical and manikin competence or practice, and understands the logistical aspects of patient care, then they are ready to face the more complicated aspects of scenarios; this involves being challenged by ‘real world’ factors (fig.1), such as environment including: light, dark, heat. The manikins being replaced by real people, delivering care whilst working at height, or in low O2 atmosphere, and so on.
So having described the 4 steps within the pre-hospital education paradigm, (technical, manikin, logistical and scenario), the authors suggest that the following are the most common mistakes made by pre-hospital educators.
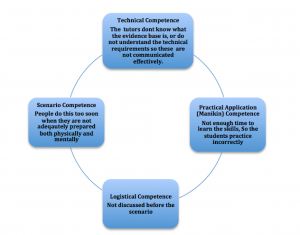
The Main Areas of Concern
The authors believe that there are some main areas of concern in this process (fig. 4):
Fig 4:The Main areas of Concern
Common Problems with Technical Competence: the Tutor (fig. 5)
Far too often in paramedic education ambulance tutors have taught what they themselves were taught, often perpetuating the myths that surround paramedic care. Cascade training is often used as the method of choice in ambulance service process changes, because it is seen as an efficient way of delivering education or training without having a negative effect upon operational cover. New pieces of equipment are introduced into ambulance services using cascade type training, with many other techniques employed that may fall short of current best practice.
Fig 5: Common Problems with Technical Competence
Cascade training is based upon the perception that training can be provided from a centre to the peripheries and that the message will stay the same; however Roberts (1998) stated that:
‘…. cascade may work if the message is strictly informational (for example about a new exam) but is liable not to work as intended if the message involves new practices based on new assumptions, theory and values.’
Hayes (2000) in a study on cascade training stated that ‘the cascade is often reduced to a trickle by the time it reaches the student (teacher)’ (p.135). In addition, Hayes commented that often the changes that are made a ‘rapid and massive’ and that this can lead to only a surface adherence to the required change, and the changes can be affected by the attitude of the student, the change itself and how it is communicated and the way in which the change is managed. Here the role of the tutor and their understanding of the skill or theory to be taught is key, and their disposition towards the required skill or change is key. Hayes (2000) described the dilution of the training and the fact that, as it is cascaded downwards, it becomes less and less understood, adding that it is not the model that is at fault but its implementation and the expertise at the top of the cascade.
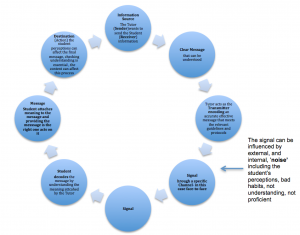
In communicating with the student the tutor should follow a simple model of communication (fig. 6) (Shannon and Weaver 1949):
The authors also believe that (Deaux et al. 1993) communication is a two way process where the sender and the receiver are responsible parties, communication needs to be interactive and the two participants must have common grounding, beliefs and assumptions that support communication. The two parties (The tutor and the student) that contribute to the process have their own expectations and understanding of the context (Riley 2008) and themselves. Here interpersonal communication occurs using negotiation between the two participants, and can be affected by a range of clinical guidelines, rules and protocols (fig.7). In addition, the tutor needs to remember that they are facilitating practice (Riley 2008) rather than teaching it; this can bring cost pressures, resources and time constraints, as tutors need to be developed to change their style from traditional teaching to facilitation.
The authors suggest that not enough attention is given by tutors to actually taking the time to understand the evidence base behind a particular skill that they are teaching, preferring to teach the information that they themselves were taught, causing classical communication and understanding issues. The pre-hospital environment is constantly evolving due to new technology and changing medical information and research., and tutors need to identify their educational needs and then, using evidence-based practice, fill any gaps that they identify. They must be encouraged to attend conferences and network; however, opportunities for paramedics to learn skills from experts in their field are often limited due to lack of active researchers in the UK.
|
The signal can be influenced by external, and internal, ‘noise’ including the student’s perceptions, bad habits, not understanding, not proficient |
Fig 6: A simple model of Communication (Shannon and Weaver 1949)
Other possible problems with Technical Competence include: not enough time being given to lesson planning or researching sessions prior to delivery; tutors using other tutor’s sessions, which they do not understand and tutors using pre- prepared instructor slide sets where they have not taken the time to actively learn or prepare their subject.
Common Problems with Technical Competence: The Student (fig 6) (click to enlarge)
The authors suggest that competence in the pre hospital arena is not just about knowledge and skills, it is about developing the ability to meet demands in complex situations that require the students to draw on psychosocial resources including skills and attitudes and the practical and communication skills required (fig. 10). The tutors need to consider not only the knowledge and skills that the student has using an individual training needs analysis approach, they need to consider the traits of the student, their attitudes (personal and social values), self-control and self-confidence. If the student does not believe they can do the task then this could impact on their performance and its sustainability, and this can impact on healthcare provision and adherence to guidelines etc.
A number of other factors inbuilt in the student, including personal motivation, can affect the broad nature, intensity and persistence of the effort (Campbell 1993); for example, students may gain competence in the ALS procedure but when in the practice setting the student may see paramedic with whom they work missing aspects of the process out, making them develop ‘short cuts’. Here the development of clear objectives and learning outcomes is paramount, as this provides the end product and the rationale behind them, and the fact that a certain process will ‘save lives’. Locke and Latham (1990) felt that feedback on practice, sufficient resources to carry out a task, clear role expectations, clear standards of performance and the implied ‘rewards’ for accuracy were key to good practice.
As experienced educationalists the authors acknowledge that no two students are alike, each will have their own individual levels of motivation and attitude and will respond differently to different methods of teaching; something the tutor needs to be aware of. The learning styles (the way the student synthesises the information taught), the approaches to learning (surface, deep and strategic) and intellectual development of the student must be taken into consideration (Ryan and Halliwell 2011, Felder and Brent 2005). That is not to say that the tutor needs to individualise the learning but that they need to be aware of the differences and adapt to meet them, using a balanced approach that can attempt to match the students’ preferences. The authors support the suggestion that students need to have (Felder and Brent 2005): a variety and choice of learning tasks to challenge their beliefs and attitudes; clear communication and an explanation of expectations; modeling, practice and feedback; a student centred learning environment where problem solving approaches are adopted and the respect of the tutors; although Riley (2008) states that this can become less organized, and so a structured approach is essential.
The student needs to have confidence in their ability and performance, in the correct amount, for good performance, as this maintains the students’ confidence when in the practice environment. The authors suggest that the overconfident, however, student presents a problem as they may not listen to instruction, refusing to acknowledge potential weaknesses and the downfalls of their attitude, and this can affect their ability to develop or improve their practice, and lead to an overestimation of their performance and ability (Kruger and Dunning 1999). Feedback on the students’ performance is key to the development of confidence, and helps to develop corrective changes; this is supported by opportunities to practice in a safe learning environment with the tutor’s guidance, supported by constructive and honest feedback on their performance and the areas requiring change and improvement.
Common Problems with Practical Application (Manikin) Competence (fig. 7) (see above)
The authors have observed that there was often not enough time allowed for the preparation phase of practical application competence. The students are introduced to scenarios resembling real life too early in the training process and this leads to student failure due to the fact that they still lack technical skills, they haven’t learned the practical competence, and they still lack the ability to put all the skills learnt into a skill set (fig, 10).
The scenarios are often planned so that they test aspects of the skill that are, as yet, beyond the student’s ability or remit, or the student has not developed enough muscle memory, and may not have had time to consolidate their skills. Furthermore, The students have often not had enough time to discuss the logistical aspects, or create mental models of practice. These issues can lead to the scenario throwing up many factors, beyond those for which the student is being prepared, and often beyond the original objectives of the scenario (Riley 2008). It is the authors’ belief that the time allocated to the practical coaching in the skill is limited, and time is often not set aside for this to be done; with tutors preferring to spend time on the underpinning theory to the detriment of practice. When the simulation requires a problem based approach, as it inevitably does in pre hospital education, the time allowed for this process to be worked through (Riley 2008) must be built into the process, and planned for, when designing the scenario.
Simulation using manikins should offer the opportunity to gain and assess skills though repeated practice in a safe environment (Kneebone 2003), and there needs to be objective measures of the skill and the ability to test the skill in a safe environment where patient safety is not at risk. Simulation should offer a safe and student-centred approach to learning through repetition practice; but it must be underpinned with knowledge and a professional attitude, as well as knowledge of how to use the simulation equipment (fig. 10). Without time to practice skills the muscle memory cannot develop (Krakauer and Shadmehr 2006), as this can only be enhanced with time and practice; in addition, the new skills need to be refreshed so they remain in the memory. The learning process should involve a two way process where the tutor provides the conditions under which understanding is possible and the student takes responsibility for the learning opportunity (Rogers 1983). In addition, there needs to be a relationship between the practical training and real life application of clinical skills, so the student can apply what they have learnt without having to ‘unpick’ it because it was too complicated or lacked reality (Kneebone 2003).
Fig 7: Common problems with Practical Application (Manikin) Competence
Common Problems with Logistical Competence (fig. 8) (see above)
The authors have found that logistical issues are often used in scenarios to create difficulty, but this can detract from the actual ability of the student to perform the skills that the scenario was actually set up to review. This area should, the authors suggest be considered in all scenario teaching, to support the student in considering and rehearsing the logistical considerations that may occur. These can be as simple as making more space around a patient, or where to place equipment at a cardiac arrest, or as complex as how to extricate a patient from a given area.
The authors recommend a 2-3 minute review of logistics with the student prior to them entering any given training scenario; with a discussion between them and the tutor about all logistical issues before the actual scenario begins using a simple question: can you envisage any logistical problems with this scene? We suggest a logistically ‘SMART’ to assist (Halliwell 2012) (fig. 10):
- Space: Can more space be created?
- Move: Can things be moved? Can the patient be moved?
- Access: How much of the patient do you need to access?
- Resources: Where are you going to place your equipment? Why?
- Transport: What will your method of transport be? What are the clinical effects of moving the patient? How will movement affect the patient’s physiological status?
Fig 8: The Logistical Stage
Common Problems with Scenario Competence (fig. 9)
From the author’s experience scenarios are often set without a clear understanding of the actual learning objective (Riley 2008). Observation of over 100 clinical scenarios captured, reviewed on video, has shown the authors that often the scenario involves the assessment of a wide range of skills beyond those that were probably intended by the designer of the scenario, including assessment of clinical skills, communication, and decision making. But in many cases the scenario fails to have the desired result due to logistical reasons, such as setting equipment up in the wrong place, or not creating space sufficient to access the patient. Pre-hospital care covers the ‘any patient, of any age with any condition, in any environment and location’ and often in scenarios students can face assessment in all of the above, which can be overwhelming for the student.
We believe that by giving the student the opportunity to think through the logistics, as one would do in a ‘seen examination’ at university, they are better able to focus on the clinical aspects of delivering higher quality care.
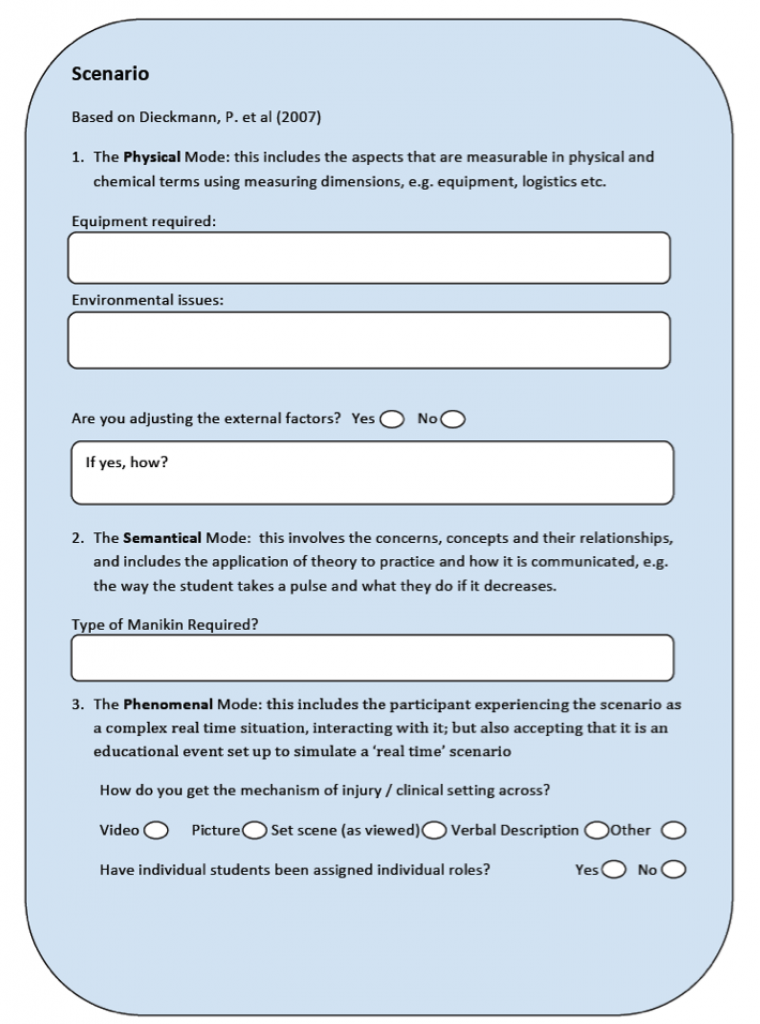
Scenario based education is very common in paramedic education, because of the practical nature of paramedicine, and fits with the principles of adult learning, Androgogy (Knowles et al. 1980). Students need to know the reason for learning a task (need to know), they need to have the theory behind the task (foundation) and they need to be involved in the planning and evaluation of the task (self-evaluation). In addition, the task needs to be relevant to their role, the scenario needs to be problem centred (orientation to their role) and the students need to be motivated to learn (motivation). Most paramedic educational schemes in the UK use several patient simulators and a range of clinical scenarios to support the gradual acquisition of the necessary skills to approach and treat patients. This highly sophisticated process of learning encourages a hands-on training experience that fully engages students in a realistic and risk-free learning environment, and matching the simulation realism to the desired outcomes is key (Dieckmann et al. 2007). Risk-free simulation sessions prepare paramedic students that can offer better patient care in the real world.
Fig 9: The Scenario Competence (see above)
Clinical scenarios support paramedic education because they focus teaching practices on individual learning and use clinical scenarios to simulate real-life environments. These scenarios are designed to allow students to provide healthcare on increasing levels of complexity. Instructors are then able to assess the performance and proficiency of each student objectively. In a recent Laerdal Medical Publication Klarian (2012) stated that:
Clinical simulation is very human. It allows a student to feel what he/she is contributing, and it enhances skills and helps to overcome difficulties in the area of soft skills: knowledge, know-how and discipline (p.2)
And felt that:
Students learn by doing and this impacts directly on the quality of healthcare, since learning in a risk-free environment contributes to and builds confidence to prepare students for their initial approach and contact with real patients (p.2)
For tutors the use of simulation and clinical scenarios involves an understanding of the intended learning outcome and experience, and should address one or more of the relevant intended learning outcomes (Riley 2008) (fig. 10: Learning Outcomes). Simulation is being used to develop students in a number of professional spheres, and many types of simulation training experiences are used throughout a variety of medical disciplines and professions. Klarian (2012) concluded that ‘As far as clinical scenario simulation is concerned, there’s no doubt about its efficiency’ (p.2). Simulation can be optimised for learning and South Western Ambulance NHS Foundation Trust and Bournemouth University surveys suggest that there is a high level of student satisfaction and enjoyment learning with simulation. Simulation, along with classroom training, prepares professionals for healthcare careers supporting the acquisition of knowledge, skills and values. When students graduate from a paramedic programme, having trained in critical and time pressured events safely, they are ready to apply what they have learnt in their work with patients. This hands-on educational model results in a higher quality of life and better public health.
Scenario Competence and the suggested application
As the Tutor develops the scenario that they will use to practice a skill and to develop the students skills and performance they need to consider all the aspects discussed above as shown in Fig 10. The scenario needs to have a more structured approach to encompass all the areas of concern as well as considering the:
- Technical Competence: ensuring that the Tutor has the evidence base required and the student has the skills, knowledge and aptitude for the scenario before they are asked to complete it.
- Application (Manikin) Competence: ensuring that the student has the time to develop the skills and coordination (muscle memory), required, and that they have been able to familiarise themselves with the equipment they will be using.
- Logistical Competence: involving the creation of space to work in, ensuring that the patient and their surroundings can be moved so that access to the patient can be gained. Knowing the correct place for the equipment being used, and how the patient will be transported.
In developing the scenario we need to consider the three modes of thinking (Dieckmann et al. 2007) (fig, 10), and to ensure that we can match the learning outcomes required to the ‘Real World’ (fig.1) including the:
- Physical Mode: which includes the things that we can measure in fundamental physical and chemical terms, e.g. equipment, logistics etc. The Tutor needs to adjust the scenario to potential external factors to provide reality in a safe setting, allowing the student to develop their skills in a number of potential reality scenarios to develop their muscle memory with the support of the Tutor.
- Semantical Mode: which encompasses
- The technical aspects
- The information provided as part of the briefing
- The student’s knowledge
- Concerns and concepts and their relationships; the application of theory to practice and the development of the decision making process (Ryan and Halliwell 2011).
This includes the theory behind the practice and how it is communicated (the way the student does things like taking a pulse and what they do if it decreases. This includes the type of manikin required and whether the student has been trained in its use.
- Phenomenal Mode: which includes the fact that the participant experiences the scenario as a complex real time situation (The Real World in fig. 1), interacting with it; but also accepting that it is an educational event set up to simulate a ‘real time’ scenario. The student is assigned their role within the scenario and feels confident about that role and the interactions involved in it, e.g. the assistant practitioner. They are able, with time, to develop their coordination (muscle memory) and hand-eye coordination, as well as their priorities about safe and unsafe, normal and abnormal; their values.
The Tutor must accept that the scenario is dynamic and will change depending on the introduction of ‘reality’ and the form that it takes, the differing learning needs and knowledge base of the of the student, the stage in the student’s learning process and so on (Dieckmann et al. 2007).
Conclusion
In bringing this paper to a conclusion the authors ask those with responsibility for paramedic education and the failure of those undertaking clinical scenarios to consider the importance of ensuring that their scenarios have been designed to achieve a specific learning outcome, and that the scenarios are designed in a manner that ensures that the student has the technical and practical skills to achieve the required outcomes. Furthermore, we stress the importance of allowing logistical considerations to become a separate area for students to discuss, and comprehend, before they undertake a clinical scenario. We believe that by allowing time for consideration of logistical considerations, and treating these as a stand-alone element of any assessment we will be able to focus on the technical and practical competence and subsequent clinical safety of those being assessed.
References
Banks, F. Barlex, D, Owen-Jackson, G. Jarvinen, E. and Rutland, M. (2000) Findings of an international teacher training research study the DEPTH Project. Available at: http://www.iteaconnect.org/Conference/PATT/PATT10/BarlexBanks.pdf [Accessed 30 August 2012].
Barrett, D. (2007) The clinical role of nurse lecturers: Past, present, and future, Nurse Education Today, vol.27, no.5, pp.367-374.
Benner, P. (2001) From Novice to Expert, Prentice Hall: New Jersey, USA
Campbell, M.D. McCloy, S.H. and Sagar, C.E. (1993) A theory of Performance, In Personnal Selection in Organisations, eds Schmitt, N. and Bormann, W.C., Josey-Bass: San Francisco.
Caroline, N. (2012) Emergency Care in the Streets, 6th edition, Jones and Bartlett: London.
Della-Maggiore, V. (2005) Motor Memory Consolidation, Night and Day, Journal of Neuroscience, vol. 25, no.40, pp.9067-9068.
Deaux, K., Dane, F.C. and Wrightsman, L.S. (1993) Social Psychology in the ‘90s, Brooks-Cole Publishing: Pacific Grove, California.
Felder, R.M. and Brent, R. (2005) Understanding Student Differences, Journal of Engineering Education, vol.94, no.1, pp.57-72
Fine, E.J., Ionita, C.C., Lohr, L. (2002) The history of the development of the cerebellar examination, Seminal Neurology, vol.22, no.4, pp.375–84.
Dieckmann, P., Gaba, D. and Rall, M. (2007) Deepening the Theoretical Foundations of Patient Simulation as Social Practice, Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, Vol.2, no.3, pp.183-193.
Hayes, D. (2000) Cascade Training and Teachers’ Professional Development, ELT Journal: An International Journal for Teachers of English to Speakers of other languages, vol.53, no.1, pp.22-27.
Howell, W.S. (1979) Theoretical Directions for intercultural communication, in Asanti, M.K, Newmark, E. and Blake, C.A. (Eds) Handbook of Intercultural Communication, pp.23-41, Sage: California, USA.
Howell, W.S. (1982) The Empathic Communicator, Wadsworth: California, USA.
Kenny, G., Pontin, D. and Moore, L. (2004) Negotiating socialisation: the journey of novice nurse academics into higher education, Nurse Education Today, vol.24, no.8, pp.629-637.
Knowles, M., Holton, E.F. and Swanson, R.A. The adult learner: the definitive classic in adult education and resource development, 6th edition, Elsevier: Burlington.
Krakauer, J.W., and Shadmehr, R. (2006) Consolidation of motor memory. Trends in Neurosciences, vol.29, pp.58-64.
Klarian, M.A. (2012) Nursing School at Universidad de las Americas (UDLA) Publication, Laerdal Medical: USA.
Kneebone, r. (2003) Simulation in surgical training: educational issues and practical implications, Medical Education, vol.37, no.3, pp.267-277.
Kruger, J. and Dunning, D. (1998) Unskilled and unaware of it: How difficulties in recognizing ones’ own incompetence lead to inflated self assessments, Journal of Personality and Social Psychology, vol.77, pp. 1121-1134.
Locke, E.A. and Latham, G.P. (1990) Work Motivation: The high performance cycle, In Work Motivation, eds Kleinbeck, H., Quast, H., Thierry, H. and Hacker, H., Ernblaum: Hillsdale, USA.
Paas, F., Renkel, A., and Sweller, J. (2004) Cognitive Load Theory: Instructional Implications of the Interaction between Information Structures and Cognitive Architecture, Instructional Science, vol. 32, pp.1–8.
Palmer, J. and Palmer, N. (2007) People Skills for Skilled People: Communication Excellence Institute, Available at: http://www.talk2cei.com/ezine/archive/vol4_num2_workplace.htm
[Accessed 30 August 2012].
Peyton, J.W.R. and Allery, L. (1998) Setting Objectives. In Peyton J.W.R. (Eds) Teaching and Learning in Medical Practice, Manticore Europe Limited: Rickmansworth.
Plato (translation Sterling, R. and Scott, W.) The Republic, Norton: New York.
Roberts, J. (1998). Language Teacher Education, Arnold: Great Britain.
Ridley, D.S., Schutz, P.A., Glanz, R.S. and Weinstein, C.E. (1992) Self-Regulated Learning: The Interactive Influence of Metacognitive Awareness and Goal-Setting, The Journal of Experimental Education,vol.60, no.4, pp.293-306.
Riley, R.H. (2008) Manual of simulation in healthcare, Oxford University Press: Oxford.
Roberts, J (1998) Language Teacher Education, Arnold: London.
Rogers, C.R. (1983) Freedom to Learn for the 80’s, Merrill: New York.
Ryan, E. and Halliwell, D. (2012) Paramedic Decision making – how is it done? Journal of Paramedic Practice, vol.4, no. 6.
Scardamalia, M. and Bereiter, C. (1991) Higher Levels of Agency for Children in Knowledge Building: A Challenge for the Design of New Knowledge Media, The Journal of the Learning Sciences, vol.1, no.1, pp. 37-68.
Shannon, C. and Weaver, W. (1949) The Mathematical Theory of Communication, University of Illinois Ptress: Urbana, Illinois.
Tomei, L. (1998). Learning theories — A primer exercise. Excerpts from Educational Psychology, a course taught by Tomei, L., Duquesne University and Applying educational psychology in the classroom, a text by Dembo, M.H., University of Southern California. Available at: http://www.duq.edu/~tomei/ed711psy/b_cai.htm [Accessed 30 August 2012].
Wolf, U., Rapoport, M.J., Schweizer, T.A. (2009) Evaluating the affective component of the cerebellar cognitive affective syndrome, Journal of Neuropsychiatry Clinical Neuroscience, vol.21, no.3, pp.245–5.
Wolpert, D.M., Diedrichsen, J. and Flanagan, J.R. (2011) Nature Reviews NeuroScience, vol.12, pp. 739 – 751.
Lance Baily, BA, EMT-B, is the Founder & CEO of HealthySimulation.com, which he started while serving as the Director of the Nevada System of Higher Education’s Clinical Simulation Center of Las Vegas back in 2010. Lance is also the Founder and acting Advisor to the Board of SimGHOSTS.org, the world’s only non-profit organization dedicated to supporting professionals operating healthcare simulation technologies. His co-edited Book: “Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice” is cited as a key source for professional certification in the industry. Lance’s background also includes serving as a Simulation Technology Specialist for the LA Community College District, EMS fire fighting, Hollywood movie production, rescue diving, and global travel. He and his wife Abigail Baily, PhD live in Las Vegas, Nevada with their two amazing daughters.
Sponsored Content: