Simulated VR Training Improves Surgical Training by 130% & Other VR Sim Updates
Moving at ludicrous speed, Virtual Reality applications are continue to make huge impacts across the entire field of Surgical Training via medical simulation. UCLA just published research showing a 130% improvement in Surgical Resident training with VR training, tactile haptic feedback research is showing promising results for physical sensation, machine-based learning algorithms for surgery performance and eye-tracking integrations also demonstrate massive adoption and innovation in the unique field. Let’s take a look at some of the most recent headline news in VR surgical simulated training.
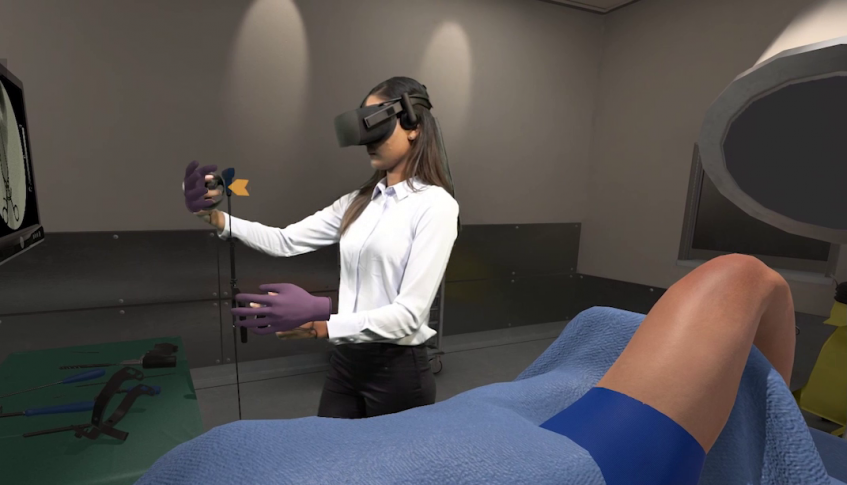
MD+DI: Osso VR Expands Its Reach, Shares Study Results: A just-released study entitled “Randomized, Controlled Trial of a Virtual Reality Tool to Teach Surgical Technique for Tibial Shaft Fracture Intramedullary Nailing” conducted by UCLA’s David Geffen School of Medicine shows that the surgical performance of Osso VR users “improved by 130% and their speed was 20% faster,” Justin Barad, MD, CEO and co-founder of Osso VR, told MD+DI. “These are not subtle differences. Research is showing that VR users are faster and more competent.” He added that just after 30 minutes of VR training, the “effect is startling.”
Such news follows Osso VR’s July announcement that its platform is now being used by more than 20 teaching hospitals as well as eight medical device companies in 11 countries. Hospitals include Brown University, Vanderbilt University, Hospital for Special Surgery, Marshall University, Newcastle Simulation Centre, The University of Hawaii, UCLA, University of Washington, Wake Forest Baptiste Health, University of Kentucky, University of Utah, and New York University.
Sponsored Content:
RY Ortho “How To Maximize Simulation Training? New Study Says Use Tactile Feedback”: A team of University of Iowa researchers studied 55 residents from four medical centers in order to determine whether simulator-based wire navigation training can transfer to higher-level tasks.
Co-author Donald D. Anderson, Ph.D., director of the Orthopaedic Biomechanics Laboratory at the University of Iowa explained the genesis of this study to OTW, “Orthopaedic residents can struggle with fluoroscopic wire navigation skills when they first enter the operating room (OR). A lack of training opportunities outside of the OR may create an unnecessary patient safety risk and yield inferior results during a resident’s first opportunity to perform this task during surgery.”
“While some skills are best learned in the OR, orthopaedic residents can enter the OR with improved skill if they first go through a validated simulation training that targets the development of specific skills. A structured simulator curriculum can facilitate deliberate practice supported by immediate, objective feedback and assessment. This underscores the fact that providing residents with a dedicated time and space for practice is key to having higher performing residents.” “A huge part of orthopaedic surgery is using tools and feeling how they interact with bone. Although virtual reality simulators have lots to offer, our belief is that having this realistic tactile feedback is essential to learning.”
Business Insider: Here’s how virtual reality is training the doctors of the future: OMS is rolling out its VR training platform to assist with medical education at the Oxford Simulation and Teaching Resource center at John Radcliffe Hospital in Oxfordshire, UK — a teaching institution for Oxford Medical School. Although still in the early stages of VR’s move into healthcare, and without definitive evidence that VR disruption can bring clinical improvements, many care providers may feel uncertain about its place in their organization. However, nearly every major tech company is already invested in a first-party extended reality platform, and the global AR and VR healthcare market is set to grow at an annual rate of 37% from 2017 to hit $5 billion in total value by 2023.
Sponsored Content:
Fundamental Surgery Now Supports the Vive Pro Eye Headset for Eye Tracking & More: Allowing Users to Have a More Seamless and Better Measured Surgical HapticVR Training Experience, the new capability will also allow users and their supervisors to collect more data around what each user is paying attention to during surgical simulations and better measure their surgical precision and overall performance. Those that use Fundamental Surgery with the Vive Pro Eye headset can now manage and explore the medical virtual space with greater ease and precision by navigating with their gaze. From taking X-rays and answering intra-operative multiple choice questions to selecting a specific tool or instrument, the new eye-tracking capability allows users to more seamlessly navigate the surgical platform.
News Medical “Machine learning-guided virtual reality simulators can be powerful tools in surgeon training”: Research from the Neurosurgical Simulation and Artificial Intelligence Learning Centre at The Neuro (Montreal Neurological Institute and Hospital) and McGill University shows that machine learning algorithms can accurately assess the capabilities of neurosurgeons during virtual surgery, demonstrating that virtual reality simulators using artificial intelligence can be powerful tools in surgeon training. Using this raw data, a machine learning algorithm developed performance measures such as instrument position and force applied, as well as outcomes such as amount of tumor removed and blood loss, which could predict the level of expertise of each participant with 90 per-cent accuracy. The top performing algorithm could classify participants using just six performance measures.
StatNews “Virtual and augmented reality can save lives by improving surgeons’ training” Opinion: Rapid advances in the development of medical devices in the 21st century are contributing to healthier lives, but bring with them a new challenge: teaching clinicians how to use these often-complicated technologies. Teaching them poorly, or failing to do it at all, can negate the potential benefits and put patients at risk of harm from devices that were intended to benefit them. Simulators are a way for surgeons to practice, but they are expensive and typically simulate only a single procedure. VR has revolutionized simulation by being more accessible, effective, and affordable. Its portability and ease of use open the door for practicing skills and techniques anytime, anywhere. All a surgeon needs is a headset the size of ski goggles and a motion controller for each hand.
Subscribe to Our Newsletter for The Latest VR Surgical Training News!
Lance Baily, BA, EMT-B, is the Founder & CEO of HealthySimulation.com, which he started while serving as the Director of the Nevada System of Higher Education’s Clinical Simulation Center of Las Vegas back in 2010. Lance is also the Founder and acting Advisor to the Board of SimGHOSTS.org, the world’s only non-profit organization dedicated to supporting professionals operating healthcare simulation technologies. His co-edited Book: “Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice” is cited as a key source for professional certification in the industry. Lance’s background also includes serving as a Simulation Technology Specialist for the LA Community College District, EMS fire fighting, Hollywood movie production, rescue diving, and global travel. He and his wife Abigail Baily, PhD live in Las Vegas, Nevada with their two amazing daughters.
Sponsored Content: